|
Dr. Armstrong focused on novel therapies
rather than established agents such aspirin and beta blocking
drugs: He discussed anti-thrombin/anti-platelet strategies and
anti-inflammatory strategies, as well as agents and multiple-drug
regimens that employ both approaches to reduce cellular damage
and inflammation associated with reperfusion procedures. In
addition, he noted agents that may have future roles in treating
patients with ST-segment elevation presentations such as stents
with new drugs, adenosine, and complement inhibitors. In summary,
he advocated a view of "pharmaco-invasive" treatment in which
different classes of drugs play an integral part in improving
the success rate of invasive reperfusion techniques.
Dr. Armstrong opened by presenting a model of contributors
to unstable coronary syndromes, including hemodynamic, hematologic,
infectious, inflammatory, lipid, and metabolic factors. He
noted that in the course of his presentation he would present
hypotheses and trial data on agents that may act effectively
as adjunctive pharmacotherapy with reperfusion techniques
through intervention on one or more contributing factors.
He said that there are four general goals for adjunctive
agents: enhancing the success rate of mechanical procedures,
minimizing their risks, protecting myocardium from ischemia
before and during a procedure, and retarding or reversing
the disease itself. He discussed 2 groups of patients with
acute coronary syndromes, those who presented with non-ST-segment
elevation and those presenting with ST-segment elevation.
First, he discussed strategies for patients with non-ST-segment
presentations. One approach to adjunctive therapy is use of
an anti-thrombin agent before or during reperfusion, or during
both periods. He mentioned one trial whose data were first
presented at the current conference (REPLACE II), in which
anti-thrombin therapy (through a glycoprotein IIb/IIIa inhibitor)
was tested as an adjunct to stent placement and aspirin use.
Although new data such as these will require time for analysis
and interpretation, Dr. Armstrong believes they support a
model in which generation of thrombin itself may be prevented
through a type of drug that can generally be described as
a "tissue factor inhibitor agent."
Abciximab is a glycoprotein IIb/IIIa inhibitor that has been
studied in published trials: Results indicate that it produces
improvement in outcome (myocardial infarction or death) when
used before angioplasty and shows an amplified, larger benefit
when continued after the procedure is completed. Although
they need to be interpreted with caution, Dr. Armstrong believes
that raw registry data showing a correlation between early
use of a glycoprotein IIb/IIIa inhibitor and decreased in-hospital
mortality should be discussed with caution, the data support
the hypothesis that this approach to therapy is promising.
He then turned to a discussion on the role of a combined
aspirin/clopidogrel regimen as an adjunct to angioplasty (cited
trials are PCI-CURE and CREDO,
latter presented at this conference), noting that the published
literature shows a 31% risk reduction 1 year after treatment
in the composite outcome of death or myocardial infarction.
As a summary to the first part of his presentation, Dr. Armstrong
put out the following as a revised guideline for care of patients
with non-ST-segment elevation syndromes: use of a glycoprotein
IIb/IIIa inhibitor, aspirin, clopidogrel, and an anti-thrombin
component as pre-reperfusion procedure adjunctive therapy.
He noted that further research will clarify the relative value
of each component, as well as the cost-effectiveness of drugs
and combination regimens.
The second part of his presentation centered on novel therapies
for use with patients presenting with ST-segment elevation
acute coronary syndromes. He discussed four therapies: use
of a stent plus abciximab, adenosine, the combination of glucose,
insulin, and potassium, or use of a complement inhibitor.
Dr. Armstrong started with use of a stent plus abciximab,
noting that the investigators of the ADMIRAL study have presented
extended results showing maintenance of advantage through
3 years of follow-up.
Adenosine has potential for reversing regions of no re-flow,
as well as decreasing risk for Q-wave myocardial infarction,
recurrent infarction, heart failure, and death. However, statistically
significant data have not yet been published, which means
its potential as an adjunct therapy is unclear.
Complement inhibitors have also been explored. Findings from
the CARDINAL program were
presented at the current conference. Although there was no
difference in the primary outcome, size of infarct, with use
of a complement inhibitor, there was a significant decrease
in mortality after angioplasty with use of the trial agent.
Such findings mandate larger trials and reopen the question
of the mechanism or mechanisms through which these anti-inflammatory
agents affect outcome.
Before closing, Dr. Armstrong noted 3 ongoing studies whose
results may bring some clarity to the question of adjunctive
pharmacotherapy: the Finesse study, which will compare abciximab-facilitated
reperfusion against reteplase and abciximab-facilitated reperfusion,
the Advance MI study, which will examine a possible role for
eptifibatide in the Emergency Room, and the ASSENT 4 study,
which will look at the role of a thrombolytic agent (in conjunction
with aspirin and unfractionated heparin) as an adjunct for
reperfusion.
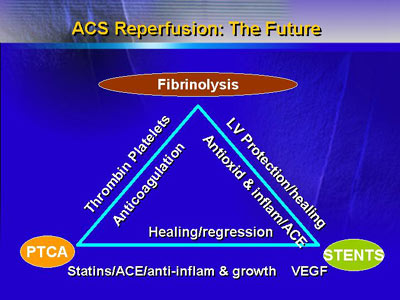
Dr. Armstrong closed with a slide that applies to reperfusion
by fibrinolysis, angioplasty, or stent placement. The sides
of the triangle represent 3 types of pharmacologic intervention:
anticoagulation, anti-inflammatory, and disease regression
(the last through agents such as statins).
|