Dr. Falkai stated that clinical evidence of progressive illness supports the hypothesis that neurodegeneration is important in schizophrenia. One study, which followed patients for three years, documented the resistance of negative symptoms to treatment. The data show a linear increase in resistance. This suggests an ongoing and worsening problem in these patients.
Another important variable is duration of untreated illness. Patients with schizophrenia have poorer outcomes and greater likelihood of relapse if the disease is not treated right away. Finally, cognitive function can deteriorate after onset of illness.
People who support the neurodevelopmental hypothesis also cite clinical progression of disease. They say it suggests that some individuals who later develop psychosis have predisposing personality traits. However, Dr. Falkai noted that these individuals are in the minority. Fewer than 10% of such individuals have schizotypal or schizoid personality traits. Furthermore, fewer than 30% of individuals who later develop schizophrenia have early behavioral precursors.
Neuropathologic studies also suggest the importance of neurodegeneration. In a postmortem study, 6 out of 33 brains from schizophrenia patients had activation of microglia compared with 0 of 23 control brains. Microglial activation is a good marker for a progressive, low-grade inflammatory process, Dr. Falkai noted.
Of course, not all neuropathologic studies have been positive. Dr. Falkai suggested researchers have been looking at the wrong parameters, such as increase in number of astroglia. For example, Parkinson's disease is clearly neurodegenerative. However, one research group found no evidence of reactive astrocytosis despite activation of microglia. Perhaps something similar applies to schizophrenia.
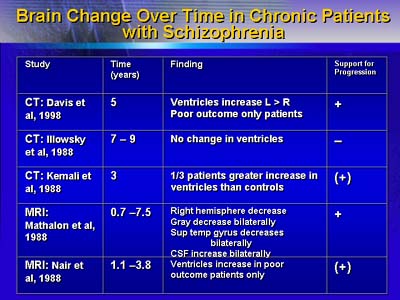
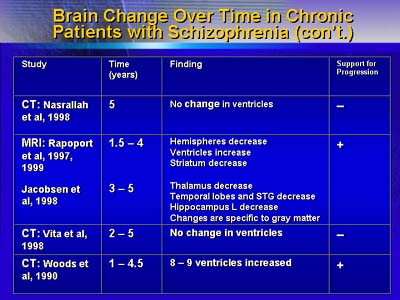
Some researchers say results from imaging studies refute the neurodegenerative hypothesis. Dr. Falkai contended that an increasing number of well-performed imaging studies support the idea of lesion progression over time. He said that Six out of nine studies have supported the hypothesis.
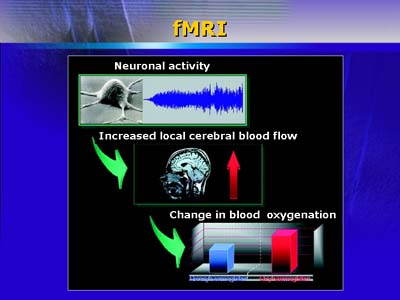
In addition, functional magnetic resonance imaging and related imaging techniques are helping researchers to understand the development of schizophrenia and treatment effect. Functional magnetic resonance imaging can give researchers an estimate of brain activation after treatment. For example, there is less activation of the right prefrontal cortex in response to haloperidol. After a change to an atypical neuroleptic, images show increased activation.
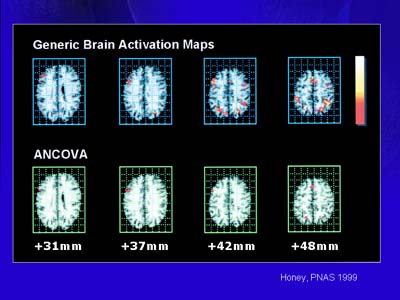
Upper row: Working memory showing fMRI-activation of the right prefrontal cortex.
Lower row: Increased activation after change to an atypical neuroleptic.
In sum, Dr. Falkai believes that the evidence suggests both development and degeneration are important in schizophrenia. He said researchers need a better understanding of how degenerative and developmental processes work together. If this is accomplished, we may find better ways to improve therapy and prevent illness.