Dr. Falkai opened by pointing out that negative symptoms of schizophrenia are principally neuropsychological, and include problems with affect, drive, and cognition, as well as disturbances of attention, executive function, and memory.
An earlier study by Liddle used cluster analysis to subdivide schizophrenic symptoms into factors of psychomotor poverty, disorganization, and reality distortion. Liddle and colleagues found an inverse correlation between the presence of negative symptoms and cerebral perfusion in the left dorso-lateral, prefrontal cortex and the superior parietal cortex. Their studies demonstrated an association between neuropsychological symptoms and cortical function.
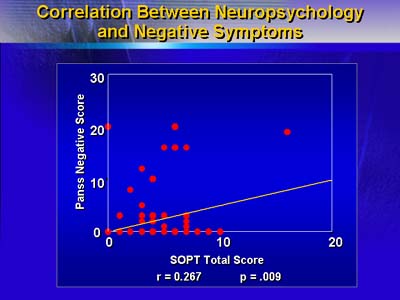
Further demonstrating that association, Falkai and colleagues used neuropsychological assessments of left frontal lobe function to demonstrate abnormalities in family members of patients with schizophrenia. Neuropsychological performance on a task that was dependent upon left frontal lobe function was directly correlated with negative symptom score on the Positive and Negative Symptom Scale for a combined group of affected and unaffected family members.
Neuroimaging studies also have suggested an association between negative symptoms and cortical function: computed tomography scans of over 200 schizophrenic patients have shown an association between negative schizophrenic symptoms and increased cerebrospinal fluid volume in cortical areas (cortical volumetric abnormalties were unrelated to positive schizophrenic symptoms). Conversely, patients with negative schizophrenic symptoms have been reported to show less volume reduction in temporal regions than do patients with positive schizophrenic symptoms.
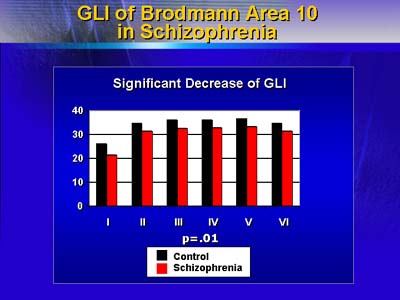
More evidence for an association between negative symptoms and cortical function comes from a study in which Falkai and colleagues examined cortical cell density in schizophrenic patients and found decreased cellular elements in Brodmann area 10 and increased cellular elements in Brodmann area 9. Having observed reduced gyrus formation in the brains of schizophrenic patients with negative symptoms and also microglial activation of the neocortex in one-third of patients with schizophrenia, Dr. Falkai speculates that schizophrenia-related cellular changes in Brodmann areas 9 and 10 may derive from a combination of neurodevelopmental and progressive processes, specifically (1) abnormal gyrus formation during the first year of life, and (2) neocortical microglial activation (as reported in neurodegenerative diseases such as Parkinson's disease).
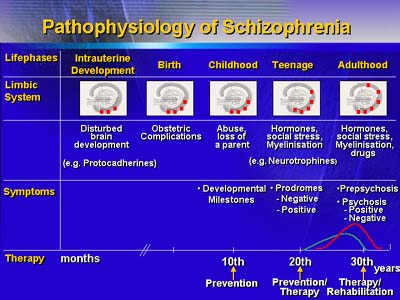
Falkai believes that neurodevelopmental and ongoing neuropathologic processes contribute to production of negative symptoms in schizophrenia.