There have been 220 studies on structural imaging in schizophrenia during the past 10 years, and their findings have sometimes differed. Dr. Sharma focused on studies using magnetic resonance imaging.
Enlargement of the lateral and third ventricles is consistent in all studies of schizophrenia. This enlargement often appears early in the illness, and may represent a pre-existing condition or a genetic marker. Findings of whole brain volume reduction have been reported inconsistently.
Reduction of frontal lobe volume has been reported in some studies. Dr. Sharma's group also found reduced volumes of the prefrontal cortex with bilateral loss of gray matter. Yet, some groups have reported enlargement of the frontal cortex. This and other inconsistencies may be due to the lack of standards for data collection or analysis, and use of different anatomic boundaries for brain regions.
Some studies have reported reduced temporal lobe volume on the left or bilaterally. This is a potentially important finding, because reduced volume of the superior temporal gyrus has been associated with "positive" schizophrenic symptoms, such as hallucinations and delusions. The volume of the hippocampus, like that of the temporal lobe, has also been reported to be reduced on the left or bilaterally.
Findings have been inconsistent about the onset and development of volumetric abnormalities in schizophrenia: some studies have detected them during the first psychotic episode, while others have not. Some researchers have suggested that volumetric abnormalities increase over the course of illness.
One study, in which caudate nucleus volumes increased during 18 months of treatment with typical antipsychotics, suggested that treatment may help reverse brain structural abnormalities in schizophrenia. This finding has been replicated. When patients were switched from antipsychotics to the benzodiazepine clonazepam, their caudate nucleus volumes decreased over the ensuing 12 months. Other than an association between brain volumetric abnormalities and poor response, structural brain volumes have little specific predictive value for medication response, according to Dr. Sharma.
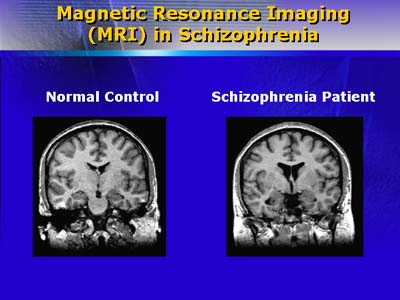
The brain of a normal control and a schizophrenia patient. The patient's brain shows marked ventricular and sulcal enlargement.
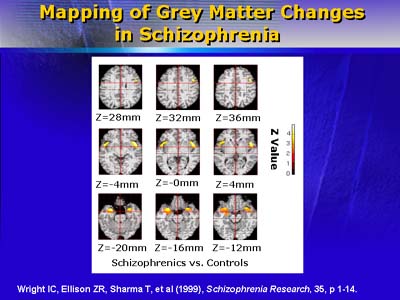
Regions of reduced grey matter in schizophrenics: Major areas of loss include right and left temporal poles and insula, right amygdala, and left dorsolateral prefrontal cortex.
One study that detected asymmetries in brains of relatives of patients with schizophrenia suggests that a genetic component may be important. Moreover, patients who have first-degree relatives with schizophrenia have been reported to have abnormalities of volume in the amygdala, cortical gray matter, and thalamic cortex. Dr. Sharma found that 80% of the siblings of a sample of schizophrenic patients had smaller brain volumes and less gray matter than controls.
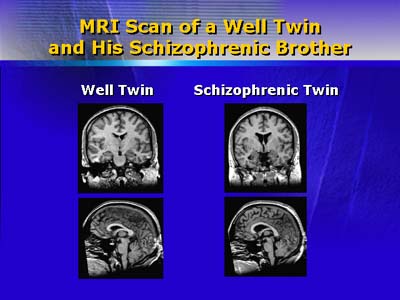
Structural brain abnormalities associated with schizophrenia are clearly shown on these MRI images. The schizophrenic individual has enlarged ventricles and cortical sulci.
These patterns prompt Dr. Sharma to believe that schizophrenia may be a disorder of structural connections. A new technique, called diffusion tensor imaging, allows visualization of axonal bundles connecting different brain regions, and may help clarify whether and to what extent abnormal connectivity may play a role in the etiology of schizophrenia.