Thioridazine prolongs the QT interval on electrocardiogram more than do other antipsychotic agents, especially haloperidol and risperidone. Therefore, thioridazine's labeling now carries extra warnings about risk of cardiovascular events.
Yet, does prolonged QT interval correlate with increased risk of cardiovascular events? According to a recent study by Dr. Hennessy and his colleagues, no clear-cut dose-response relationship exists between degree of QT prolongation and ventricular arrhythmia and/or sudden death.
To evaluate cardiovascular risk, Dr. Hennessy and colleagues used U.S. records to retrospectively evaluate cardiovascular events in 95,000 schizophrenic patients over a 30-day period of treatment with one of three antipsychotic drugs: thioridazine, haloperidol, and risperidone. They also identified cardiovascular events in a subgroup of clozapine-treated patients over a 7-day period.
They found 91 episodes of ventricular arrhythmia or cardiac arrest, (1.2 events/1,000 patient-years)-a rate within the range of that reported for other drugs.
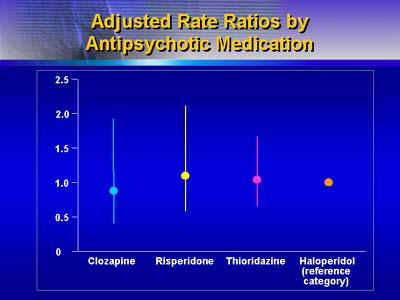
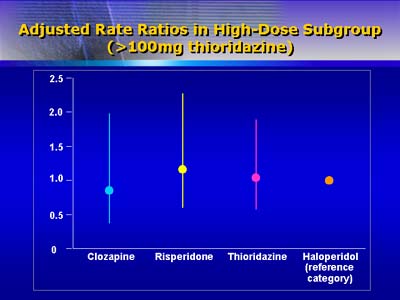
Risks of ventricular arrhythmia or sudden death were similar for all drugs studied, and were unrelated to drug dosage. Rates of cardiac events were similar for patients taking low, medium, high, and very high dosages of thioridazine.
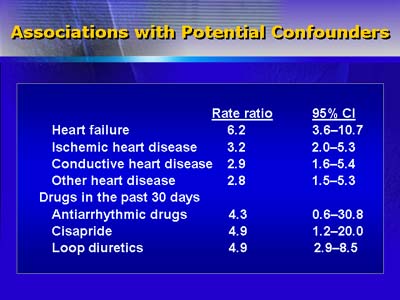
Risk factors associated with ventricular arrhythmia or sudden death included heart failure, ischemic heart disease, other heart disease, and use of antiarrythmic drugs, cisapride, or loop diuretics during the previous 30 days.
Acknowledging that their findings may be limited and that one or more confounding factors may have been missed, Hennessy and colleagues nevertheless point out that the absolute rate of cardiac events they observed and the risk factors they identified were similar to those reported in other studies.