Dr.
Byrne reported findings of a survey of behavioral and psychological
symptoms of dementia (BPSD) in clinical practice in Europe.
Apathy was the most common symptom. The survey questionnaire
examined BPSD in the context of caring, and included symptoms
that are not addressed in other BPSD measures.
The symptoms of BPSD are
a common cause of distress to patients and their caregivers.
However, what constitutes BPSD differs according to various
classification systems and guidelines. The standard measure
of BPSD is the Neuropsychiatric Inventory (NPI). However,
this measure does not address the qualitative aspects of BPSD,
such as the time of occurrence or the consequences of the
unwanted behavior. Thus, there is a danger that clinicians
will see only the behavior, ignoring the dynamic aspects of
that behavior in the patient.
To address these concerns, the European Alzheimer’s
Disease Consortium (EADC) conducted a survey of BPSD in clinical
practice. The survey population included patients and caregivers
from 12 centers in Europe.
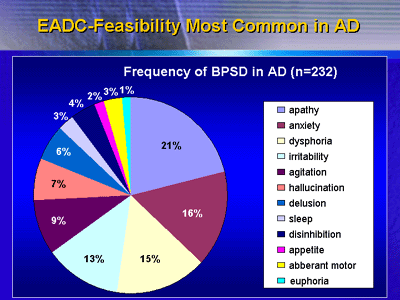
Of 698 patients entered, 368 (52.7%) had Alzheimer’s
disease. Of that group, 232 (63%) had BPSD. By comparison,
Lyketsos et al. published a U.S. investigation in 2002 called
the Cardiovascular Health Study. For all dementia patients
in this study, 62% had clinically significant neuropsychiatric
symptoms as defined by the NPI.
According to the results of the EADC survey,
the most common BPSD symptoms in the 232 Alzheimer’s disease
patients with BPSD included apathy (21%), anxiety (16%), and
dysphoria (15%). Sleep was relatively uncommon (3%). In contrast,
Lyketsos and colleagues found sleep symptoms to be more common
(13%). However, the magnitude of the apathy measure was similar
(18%). Dr. Byrne said investigators expected some difference
in prevalence, since the populations were not identical. Thus,
the relative frequency of any BPSD symptom appears to depend
very much on the population under study.
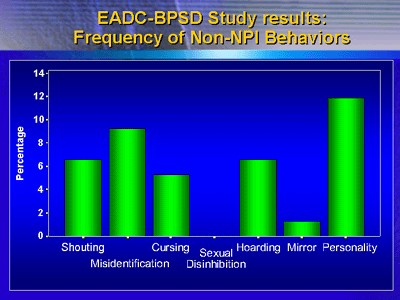
The survey results included some behaviors
and symptoms that are not included in the NPI. Changes in
personality were quite frequent, as were misidentification,
shouting and hoarding.
The EADC survey also looked at duration of
symptoms. They found that 50% of the subjects did not present
to clinicians until 2 to 5 years after symptom onset. Dr.
Byrne said this is worrying, since investigators consider
early diagnosis to be important. For the subset of patients
with Alzheimer’s disease, a somewhat smaller percentage of
patients (45%) presented 2 to 5 years after symptom onset.
The EADC researchers asked not only about
frequency and duration of BPSD, but also about the qualitative
aspects of BPSD.
About 34% of responders said that BPSD symptoms
were a problem in the daytime, while 20% said the symptoms
were not time-specific. About one-third said the behaviors
are a problem in the home, while 47% said the behaviors were
not specific to any place. The behaviors were a problem to
30% patients and 44% of caregivers.
Investigators asked what starts the behavior,
but in most cases (70.9%) responders could not identify a
trigger. However, a few cited tiredness (6.3%) and being left
alone (3.8%).
The consequences of BPSD included impairment in activities
of daily living (16.5%) and depression, anxiety or tiredness
(13.9%).
Dr. Byrne said the effect on the mood of the
patient is a notable finding. Previously, there was data showing
that BPSD affect the mood of the caregiver. Now, the EADC
provides preliminary data that these behaviors can also affect
the mood of the patient.
For the future, EADC researchers hope to elucidate
cross-cultural differences in BPSD in North, South and Mediterranean
Europe. They are also interested in conducting intervention
studies, particularly with regard to apathy.
|