|
|
Summary: The incidence of lung cancer continues to increase, yet cure rates have remained at 10-13%. Lung cancer is the most common cause of cancer death in the U.S. Dr. Sause discussed the three modalities used to treat non-small cell lung cancer: surgery, radiation therapy, and chemotherapy.
Surgery is the most effective treatment for surgically resectable cases of bronchogenic carcinoma. Patients with compromised pulmonary function and Stage I tumor may do well with limited resection, but Dr. Sause cited data indicating that patients who can tolerate a lobectomy should have this procedure due to its lower local recurrence rate. 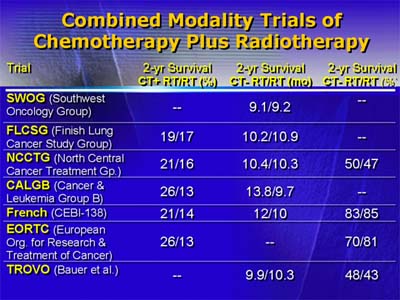
Patients with Stage II or III disease generally have marginally resectable tumors. Although postoperative radiation reduces tumor bulk, it is unclear whether it confers any survival benefit. Dr. Sause hypothesized that postoperative radiation improves local control, but ultimate failure is due to distant disease. If so, he noted, improvements in systemic treatment may make postoperative radiation more valuable. Adjuvant chemotherapy for this group of patients is controversial. Although one meta-analysis suggested a small benefit from cisplatin chemotherapy, none of the prospective, randomized trials detected any benefit. Patients with medically inoperable tumors should have radiation therapy. Postradiation survival for this set of patients is correlated with the size of the primary tumor. Dr. Sause cited a 5-year survival rate of roughly 38% for lesions smaller than 2 cm, 22% for lesions 2-3 cm, 5% for lesions 3-4 cm, and 0% for lesions larger than 4 cm. 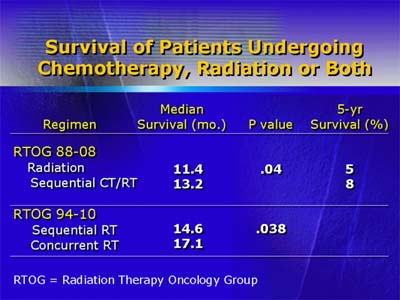
Patients with Stage III disease make up 20-30% of patients with non-small cell lung cancer. The most predictive factor for outcome is involvement of the mediastinal nodes and whether involved nodes are ipsilateral or contralateral. Large trials are underway to explore whether induction therapy with chemotherapy or chemotherapy and radiation improve survival compared with surgery alone. Patients with clinical T4 or N2 disease or both are generally considered to be surgically unresectable. Lower-staged tumors and squamous cell histology have a better prognosis. There appears to be a dose-response relation in patients who respond to radiation therapy: More aggressive radiation (with cumulative dose 45-50Gy) seems to confer survival advantage. Hyperfractionation of radiation with higher total doses may give additional benefit to responders. Studies have looked at chemotherapy combined with radiation with inconclusive results. Dr. Sause concluded that induction chemotherapy followed by radiation may enhance median and one-year survival compared with radiation alone. One study also suggests that concurrent chemotherapy-radiation is more successful than chemotherapy followed by radiation. Last, Dr. Sause discussed patients with Stage IV disease. Although study results are also inconclusive with this group, he asserted that chemotherapy in addition to best supportive care may benefit survival slightly. Certainly, the next decade will see a number of studies completed that may shed light on better treatment plans for patients with non-small cell lung cancer.
|
| Reporter: Elizabeth Coolidge-Stolz, M.D. |

