|
|
Summary: Over 23,000 new cases of ovarian cancer are diagnosed in the U.S. each year. Only about one third of patients with epithelial cancers present with localized (Stage I or II) disease. Comprehensive surgical staging is crucial for documenting diagnosis, providing optimal therapy, and defining prognosis. Women with early-stage disease can be categorized as low or high risk based on surgical and pathological findings. Dr. Gershenson addressed issues surrounding adequate surgical staging and the role of adjuvant therapy for patients at high risk for relapse.
In the U.S., ovarian cancer is the second most common cancer of the female genital tract, with an annual incidence of over 23,000 cases. Only about one third of patients with epithelial ovarian cancers present with localized (Stage I or II) disease. Surgery remains the cornerstone of treatment, determining correct diagnosis, providing optimal therapy, and defining prognosis. Dr. Gershenson stressed that incomplete staging is a major concern. One study found that only 54% of 291 patients with ovarian cancer received full staging procedures. Another study found that staging after one or two laparotomies was complete in only 53% of 86 patients. In the second study, the most frequently omitted steps during surgical staging were biopsy of the paracolic gutter or pelvic peritoneum and sampling of the retroperitoneal lymph nodes. 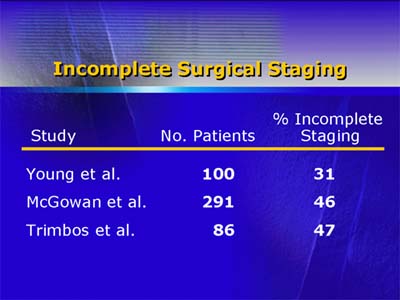
Dr. Gershenson addresses the quandary facing specialists who are referred a patient with apparent Stage I disease who has had incomplete staging. He feels that it is vital to have full staging in order to make the best decisions regarding postoperative therapy. Thus, reoperation is an option that needs to be considered seriously for this subset of patients. 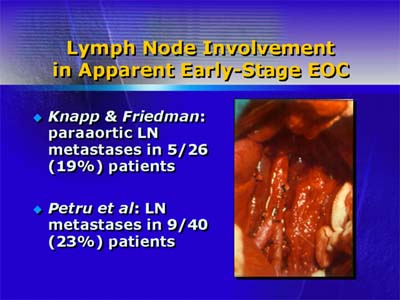
One subset for whom accurate, complete staging is critical is young patients with Stage IA disease who might be managed with preservation of reproductive potential. In one retrospective study, researchers identified 16 patients under age 40 years who had preservation of the uterus and contralateral ovary at the time of surgical staging. Patients who had high-risk factors were given adjuvant platinum-based chemotherapy. With a median follow-up of 66 months, 14 of the original 16 patients were alive without evidence of disease: Of the 14, 5 women had a total of 8 successful pregnancies, and 2 of them had undergone chemotherapy. The other 2 patients had experienced recurrent disease in the contralateral ovary and had died from their disease. 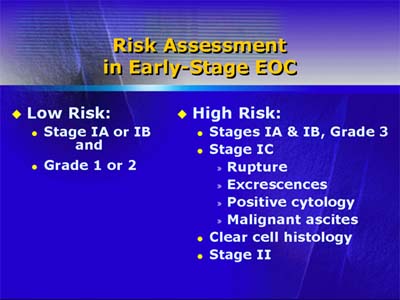
Thus, risk assessment for relapse is critically important. Within Stage I, histologic grade is the most powerful predictor of outcome. Based on other factors, low-risk early-stage epithelial ovarian cancer patients have Stage IA or IB and grade 1 or 2 disease. (Some oncologists consider grade 2 to be high risk.) High-risk patients have one or more of the following factors: (1) Stage IC or Stage II disease; (2) grade 3 disease; (3) clear-cell histology. The high-risk early-stage patients are the focus of trials of adjuvant therapy. No adjuvant therapy regimen studied in a protocol setting has yet shown a survival advantage with early-stage epithelial ovarian cancer. Ongoing and future trials may enable physicians to better define the subset of patients who require adjuvant therapy and discover and define optimal adjuvant therapies.
|
| Reporter: Elizabeth Coolidge-Stolz, M.D. |

