|
|
Summary: Despite surgical advances, rectal cancer is associated with risk of local or regional failure in patients with transmural tumors or positive nodes. Preoperative adjuvant therapy depends on clinical staging and need for sphincter preservation. Postoperative therapy depends on pathologic stage. Dr. Minsky discussed the role of adjuvant therapy, as well as trials of adjuvant regimens including newer chemotherapeutic agents. Despite radical resection, rectal cancer is associated with significant risk of local or regional failure for patients with transmural tumors or positive lymph nodes. Preoperative adjuvant therapy depends on clinical stage and need for sphincter preservation. Postoperative therapy depends on pathologic stage. Among patients who do not receive preoperative or postoperative adjuvant therapy, the incidence of local failure correlates with pathologic stage: less than 10% with stages T1-2N0M0, 15-35% with stages T3N0M0 and T1N1M0, and up to 45-65% with stages T3-4N1-2M0. Because local failure can be severely debilitating and salvage therapy is of modest success, any decrease in local failure is a clinical gain. Some surgeons assert that adjuvant therapy is unnecessary if total mesorectal excision is done: Local failure rates have been reported of roughly 5%. Dr. Minsky noted that these studies involved patients without lymph node involvement. One study reported a local failure rate of 8%, but it was 23% when patients with positive nodes were included. Dr. Minsky feels that the greatest increases in efficacy are likely to be made with improvements in integrated-modality therapy (adjuvant therapy). In the U.S., most patients who receive adjuvant therapy do so postoperatively because of the results of pathologic staging. There is controversy over postoperative adjuvant regimen. If 5-fluorouracil is used as a single agent, it should be given with continuous infusion. Otherwise, Dr. Minsky noted that all 5-fluorouracil-based regimens are of roughly equal efficacy, and selection should be based on acute toxicity profile and patient compliance. Phase II and III trials are examining newer chemotherapeutic agents such as uracil tegafur (UFT)/leucovorin, capecitabine, and oxaliplatin in combination with radiation therapy. 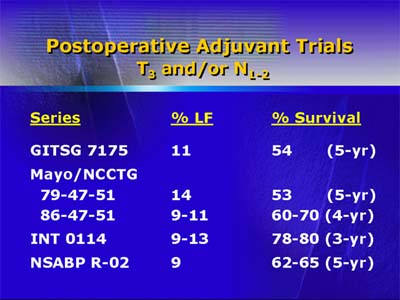
Preoperative adjuvant therapy is usually chosen when sphincter preservation and lower risk of acute toxicity are primary factors. One trial with T3 rectal cancer indicates preoperative therapy is associated with lower acute toxicity and no increase in postoperative complications. A potential disadvantage with preoperative therapy is overtreating patients with either pT1-2N0 or metastatic disease, but improved imaging techniques may lower the risk of preoperative overtreatment. 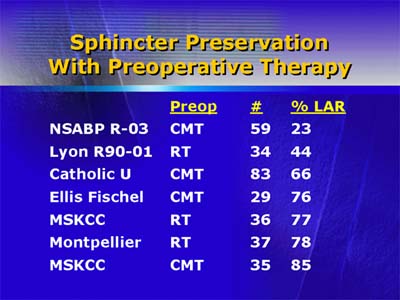
A literature review on sphincter-sparing resection indicates preoperative radiation-chemotherapy allows sphincter preservation in about 75% of patients judged clinically to require abdominal-perineal resection. A number of Phase I and II trials are underway to assess preoperative regimens with agents such as uracil tegafur (UFT)/leucovorin, oxaliplatin, eniluracil, and capecitabine.
|
| Reporter: Elizabeth Coolidge-Stolz, M.D. |

