Recent studies on improving treatment adherence in schizophrenia
demonstrate a reciprocal interaction between medication and psychological
interventions. Medication factors affecting treatment adherence
include using depot (long-acting) formulations and attempting to
minimize adverse effects by use of atypical antipsychotics.
Psychosocial interventions that may improve treatment adherence
include case management, education, and behavioral skills training.
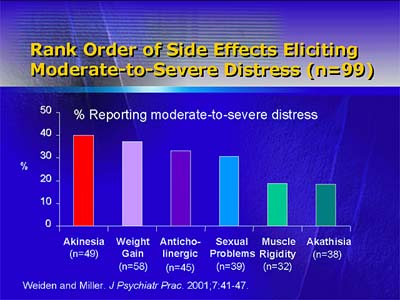
An early study of adherence behavior indicated that 46% of the patients
took less antipsychotic drug than prescribed. It is now well documented
that reluctance to take antipsychotic medication is associated in
part with extrapyramidal side effects, especially akathisia.
In clinical practice, a patient's outcome on antipsychotic medications
is largely influenced by the adverse effects experienced. These
subjective responses do not necessarily correlate with objective
physical findings. Even so, they should be treated with great care
because they can jeopardize medication adherence and interfere with
social adjustment and/or participation in psychosocial treatment.
In order to detect subjective side effects, clinicians should carefully
ask patients about any distress they experience from medication.
In most cases, akinesia and akathisia are more distressing than
tremor, rigidity, and dyskinesia.
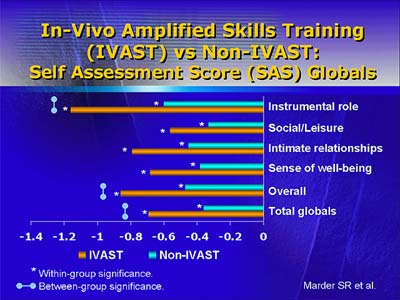
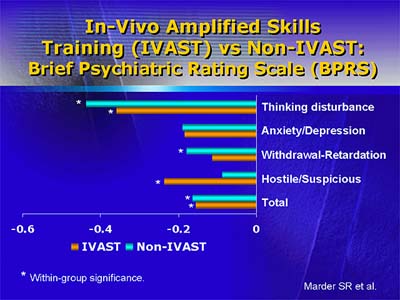
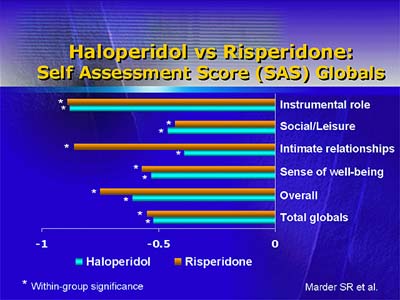
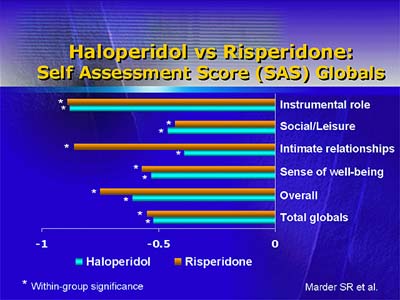
In a previous study by Dr. Marder and his colleagues, patients
were assigned to a program that supplemented skills training with
weekly sessions designed to promote the use of newly acquired skills
in the community (IVAST: in vivo amplified skills training). Patients
were also randomly assigned to a double-blind comparison of risperidone
versus haloperidol.
Brief Psychiatric Rating Scale scores showed greater improvement
with risperidone than with haloperidol in ratings of anxiety/depression.
Both risperidone and enhancement of skills training contributed
to patient satisfaction with medication and longer retention in
treatment. Akathisia also affected outcome. Patients without akathisia
who underwent in vivo amplified skills training showed the best
outcome.
In addition, medication and psychosocial strategies were shown
to interact in a one-year, double-blind comparison of clozapine
and haloperidol. Clozapine-treated patients were more likely to
participate in psychosocial programs.
Dr. Marder closed by noting that improving treatment adherence
in schizophrenia requires attention to mediating factors such as
subjective response, understanding of the illness, and side effects.
These factors are affected by both pharmacological and psychosocial
interventions, which reinforce each other.