Recently, clinicians and researchers have linked use of antipsychotic agents in schizophrenic patients with disturbances in glucose metabolism, such as new-onset hyperglycemia or Type 2 diabetes. The nature of the correlation is not clear.
Dr. Henderson discussed two studies that examined the impact of atypical antipsychotic drug use on glucose metabolism in persons with schizophrenia and drew conclusions from the data thus far available.
In one study, he and his colleagues reviewed medical records of schizophrenic patients treated with clozapine for baseline data regarding glucose metabolism. Patients with a diagnosis of diabetes prior to initiation of clozapine or who did not have baseline data recorded in their charts were excluded. Participant patients were followed for five years. Data were obtained every six months on clozapine dose, presence of absence of valproate use, and blood test results for fasting glucose and lipid profile.
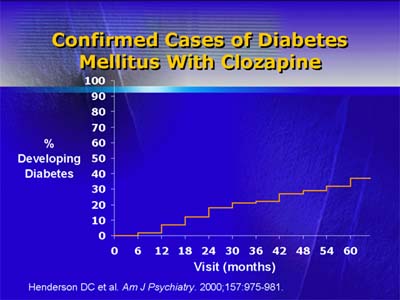
Dr. Henderson and his colleagues found that 30 of 82 patients taking clozapine developed diabetes after the initial six-month period of follow-up. Onset of diabetes was not correlated with body mass index or weight gain, but it was correlated with an increase in triglyceride level. Significant weight gain was seen in the group as a whole until roughly month 46, and the increase in weight was correlated with change in either cholesterol or triglycerides. There was a significant increase in triglycerides overall, but not a significant increase in cholesterol.
Bergman's minimal model studies glucose regulation through frequent sampling intravenous glucose tolerance testing. The methodology provides accurate depiction of the actions of insulin and glucose in normalization of plasma glucose after an injection of glucose. In this setting, measures of insulin sensitivity and glucose utilization have been extensively validated.
In the second study, Dr. Henderson and colleagues enrolled non-obese schizophrenic patients taking clozapine, risperidone, or olanzapine (with obesity defined as body mass index not more than 30 kg/m2). They excluded patients treated with anticonvulsants (namely, valproate), oral contraceptives containing norgestrol, steroids, weight loss-inducing agents, or anti-inflammatory drugs. Substance abuse, significant medical illness, and diabetes mellitus were also exclusion criteria.
There were no differences in glucose utilization comparing any two of the three drugs studied. There was a statistically significant difference in insulin sensitivity between clozapine and risperidone and between olanzapine and risperidone: Both clozapine and olanzapine were correlated with a significant decrease in insulin sensitivity. In addition, preliminary data suggest that patients on clozapine have an increased incidence of diabetes.