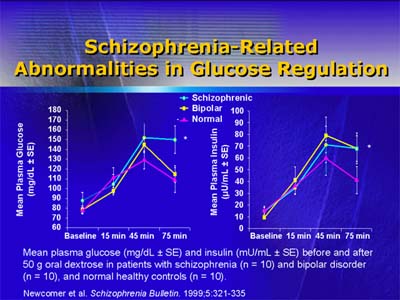
Abnormalities in glucose regulation, including Type 2 diabetes mellitus, are more common in schizophrenic persons than in the general population. Older antipsychotic drugs have been reported to exacerbate diabetes and to be associated with development of glucose disturbances or Type 2 diabetes.
So too have the newer atypical antipsychotics clozapine and olanzapine.
Case reports have described new-onset glucose abnormalities in clozapine- or olanzapine-treated patients, of whom a high proportion developed diabetic ketoacidosis, 10 (14%) of 72 clozapine-treated patients and 14 (17%) of 82 olanzapine-treated patients, on olanzapine.
Fewer case reports have described glucose abnormalities in patients taking risperidone or quetiapine (1 and 2 patients, respectively).
The rates of drug-related glucose abnormalities overall or for any individual drug are unknown.
Although rare, diabetic ketoacidosis is important because of its considerable morbidity and mortality. Even under optimal conditions (early presentation to emergency care and adequate medical treatment), the mortality rate for ketoacidosis is 2% or greater.
Persons with schizophrenia may not access medical care promptly or be able to give a clear history.
Moreover, many symptoms associated with diabetic ketoacidosis are nonspecific, such as shortness of breath, abdominal pain, and central nervous system depression, which further complicates diagnosis.
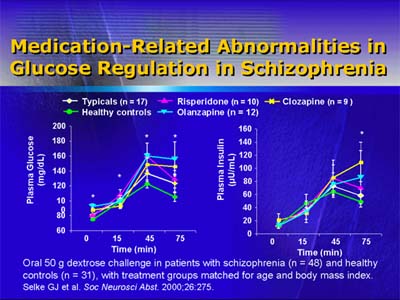
Dr. Newcomer ended with a discussion of antipsychotic agents and glucose abnormalities. He pointed out that direct effects of glucose regulation may interact with increased weight to aggravate any glucose abnormality.
Direct drug effects on glucose metabolism, in combination with drug-related changes in lipids, may increase risk for cardiovascular disease, he added.
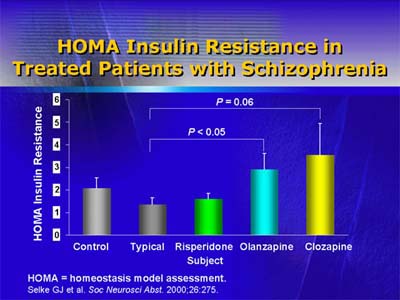
Dr. Newcomer recommended that physicians monitor antipsychotic-treated patients for hyperglycemia, changes in blood lipid concentrations, and weight gain. He recommended education of patients, families, and clinicians to reduce the risk of antipsychotic-related diabetic ketoacidosis.
Finally, he recommended collaboration between psychiatrists and endocrinologists or primary care providers.