Type 2 diabetes mellitus is a chronic metabolic disorder that is a major American public health concern because of its considerable morbidity and its high prevalence (estimated at 6% of the population at large and 10-12% of persons ages 40 years and older).
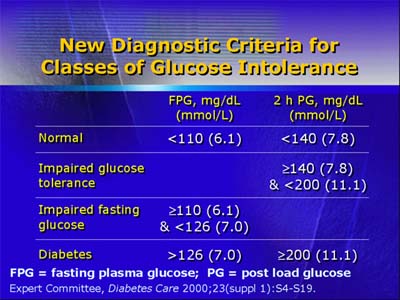
An American Diabetes Association report published in 2000 updated diagnostic criteria: (1) casual plasma glucose of at least 200 mg/dL (11.1 mmol/L) in symptomatic patients, (2) fasting plasma glucose of at least 126 mg/dL (7.0 mmol/L), or (3) 2-hour plasma glucose of at least 200 mg/dL (11.1 mmol/L) in a 75g oral glucose tolerance test.
Although susceptibility to Type 2 diabetes is a polygenic trait, environmental factors such as increased age, obesity, inactivity, and medications play a major role in the development of clinical disease.
Components of metabolic disturbance include not only insulin resistance and relative insulin deficiency, but also lipid changes (increased triglycerides and decreased high-density cholesterol), and hypertension.
Morbidity includes acceleration of atherosclerosis and development of microvascular disease in organs such as the eyes and kidneys.
Dr. Lebovitz described a number of known pathways by which medications can cause insulin resistance. They include increased appetite and caloric intake leading to obesity (or greater obesity), interference with insulin action cascade, and an increase in free fatty acid release from adipose cells. In addition, drugs can interfere directly with function of beta cells (the insulin-producing cells in the pancreas) or initiate destruction of beta cells.
All of these effects can contribute to development of Type 2 diabetes.
Recently, some case reports have correlated the use of the antipsychotic agents called atypical antipsychotics with development of diabetic ketoacidosis, an acute complication of profound insulin deficiency that carries a mortality rate of 2-4%, even when identified and treated early in its progression.
Dr. Lebovitz recommended monitoring patients who take atypical antipsychotic drugs and have risk factors for Type 2 diabetes.
Monitoring should include (1) periodic weight check with intervention if weight increases and (2) measurement of baseline fasting plasma glucose and lipids, with follow-up testing at 6 weeks and every 3 months afterward.