| Investigators
compared ticlopidine and a newer agent, cilostazol. They found cilostazol
was inferior to ticlopidine in preventing stent thrombosis. Investigators
said physicians should use ticlopidine prior to stenting of the patient
to prevent subacute thrombosis.
Subacute thrombosis can be a serious problem after stent implantation.
Physicians often use ticlopidine to help prevent or treat subacute
thrombosis after intracoronary stent placement. A newer agent physicians
can use to prevent thrombosis is cilostazol, a quinolone derivative.
Both agents are potent antiplatelet agents, but few data show
whether one is more effective than the other in preventing stent
thrombosis or angiographic outcomes.
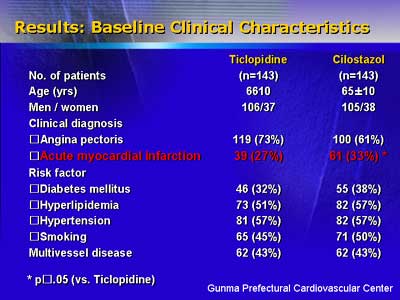
To evaluate the relative efficacy of these drugs, investigators
randomized 286 consecutive patients to aspirin(81mg/day) plus ticlopidine(200mg/day)
or aspirin(81mg/day) plus cilostazol(200mg/day). Patients received
treatment starting two days before stenting, and continuing for
six months after the procedure.
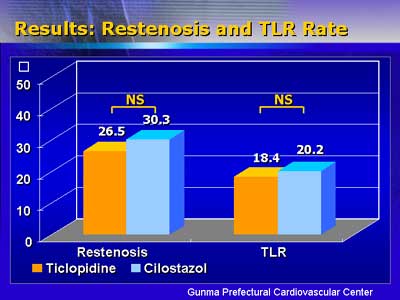
There was no statistical difference in rate of angiographic restenosis
between the two arms (26.5% for ticlopidine and 30.3% for cilostazol.)
Likewise, there was no statistical difference in rate of target
lesion revascularization (18.4% for ticlopidine and 20.2% for cilostazol.)
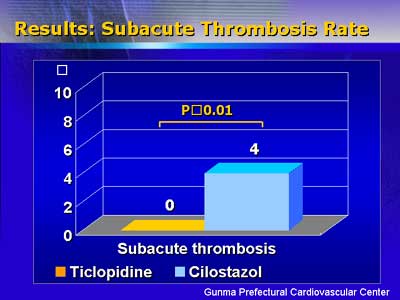
However, there was significantly more subacute thrombosis after
stent placement in the cilostazol group. None of the patients who
received ticlopidine had subacute thrombosis after stent placement,
compared with 4.2% of patients who received cilostazol.
Patient baseline characteristics were not different between groups,
although the rate of acute myocardial infarction was significantly
higher in the cilostazol group (43% versus 27% for ticlopidine.)
These investigators concluded that patients who receive coronary
stents are more likely to benefit from ticlopidine prophylaxis.
In particular, they said physicians should use ticlopidine prior
to stenting to prevent subacute thrombosis.
|