|
In this follow-up analysis of CAPRICORN,
investigators found that carvedilol improves clinical outcome in
patients with left ventricular dysfunction after acute myocardial
infarction. These findings were consistent regardless of patient
age, sex, history of angina, and other factors. These findings suggest
high-risk patients with left ventricular dysfunction will benefit
if this beta-blocker is included in post-myocardial infarction therapy.
Previous studies have shown that beta blockade after myocardial infarction
provides long-term benefits including reduced rates of mortality,
sudden death and non-fatal reinfarction. However, investigators conducted
these trials in the treatment era before thrombolysis and angiotensin-converting
enzyme inhibitors. Furthermore, they did not measure left ventricular
function and typically excluded heart failure patients.
Dr. Sharpe presented new data regarding carvedilol efficacy on morbidity
and mortality in left ventricular dysfunction patients who had a myocardial
infarction. They treated these patients according to a protocol that
required use of an angiotensin-converting enzyme inhibitor.
The data comes from the double blind, randomized, placebo-controlled
CAPRICORN trial. This trial included nearly 2,000 patients with acute
myocardial infarction and a left ventricular ejection fraction of
40% or less. Almost all of them received angiotensin-converting enzyme
inhibitors.
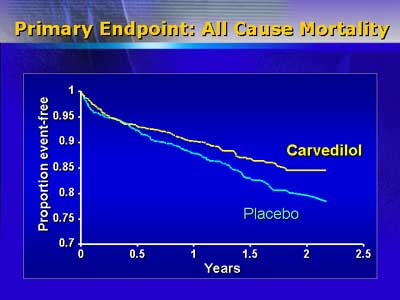
As reported in May 2001 in The Lancet, carvedilol reduced all-cause
mortality by 23% (from 15% to 12%). The beta-blocker also reduced
the composite of all cause mortality and cardiovascular hospitalizations
by 8%. These were the primary endpoints of the study.
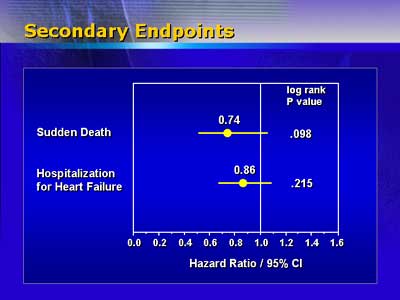
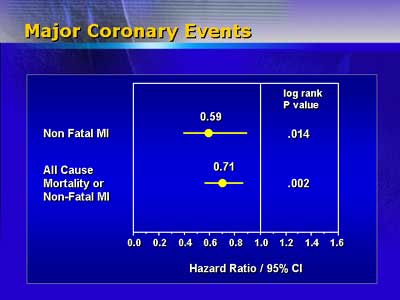
In an oral presentation, Dr. Sharpe revealed that carvedilol also
reduces cardiovascular mortality by 25% (from 14% to 11%). Recurrent
myocardial infarction was halved from 6% to 3%.
The combined endpoint of all major cardiovascular events (cardiovascular
death, non-fatal myocardial infarction, hospitalization for heart
failure) was 19% lower in the group of patients treated with carvedilol.
Patient benefit was consistent regardless of age, sex, ejection fraction,
location of myocardial infarction, previous history of angina or myocardial
infarction, presence of diabetes or heart failure, and other factors.
In addition, Dr. Sharpe reported that treating 43 of these high risk
left ventricular dysfunction patients would prevent one death per
year. The number needed to treat for ACE inhibitors alone is similar
to this in this patient group, but in CAPRICORN this benefit was additive
to the ACE inhibitor benefit.
One attendee asked whether these findings suggest a class effect
for beta-blockers in this patient population. Dr. Sharpe did not
rule out this possibility, but noted that data is available only
to support the use of carvedilol in this situation.
CAPRICORN Sub-study Results:
| |
Carvedilol
|
Control
|
|
All cause mortality
|
12 %
|
15 %
|
|
Cardiovascular mortality
|
11 %
|
14 %
|
|
Recurrent myocardial infarction
|
3 %
|
6 %
|
|