| Dr. Tracy took
a population-based approach to his discussion of correlation of markers
of inflammation with risk for cardiovascular disease. He mentioned
three types of markers: systemic ones including C-reactive protein
and fibrinogen, systemic and local mediators, and cell adhesion markers.
Most of his discussion centered on C-reactive protein. He concluded
that many biomarkers may be valid risk predictors and the choice for
clinicians may depend more on technical factors such as standardization
and sensitivity and specificity than correlation of marker and risk
for cardiovascular disease.
Dr. Tracy took a population-based approach, citing studies that
have examined possible biomarkers of inflammation such as systemic
markers, systemic and local mediators, and cell adhesion markers.
His focus was largely on C-reactive protein. However, he asserted
that final choices of marker(s) for use in the clinical setting
will probably depend more on technical factors such as standardization
and sensitivity and specificity than the validity of the association
between an individual marker and cardiovascular risk.
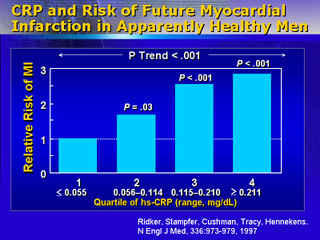
He discussed two prospective studies on C-reactive protein level
and cardiovascular disease. In one study, C-reactive protein levels
were obtained from healthy young adults. Ten years later, subjects
were screened for coronary calcifications. Individuals who had ranked
in the third quartile for protein level at year five were twice
as likely to have evidence of calcification. In a study of older
men, ranking in the highest quartile for C-reactive protein predicted
a three-fold increase in short-term risk for myocardial infarction
compared with risk for subjects in the lowest quartile.
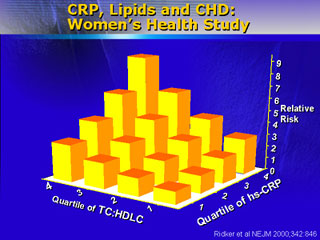
The C-reactive protein biomarker is valid for relative risk for
signs of atherosclerosis (calcification in younger adults, infarction
in older people), but it reflects only the inflammatory aspect of
the disease. If lipid-related risk is charted on one axis, the protein
on a second, and relative risk on the third (vertical) axis, a depiction
is obtained that Dr. Tracy feels is probably most valid in presenting
relative risk. Analysis shows that 0 risk is obtained at lipid levels
of roughly 140 total cholesterol and 80 LDL cholesterol. Maintenance
of such levels in mice does result in suppression of atherosclerosis.
Because researchers do not understand the biology underlying the
association between lipids, inflammatory markers, and cardiovascular
disease, they look for correlations between known risk factors and
biomarker elevation. Elevated C-reactive protein levels have been
correlated with numerous risk factors. General correlation with
metabolic disorders including hypertension, hyperglycemia, and obesity,
as well as correlation between degree of elevation and number of
metabolic disorders present in an individual, has several implications.
First, markers in older people, who have a higher likelihood of
comorbidity along with cardiovascular disease, are more likely to
be nonspecific for cardiovascular disease. Second, change in marker
level over time may reflect development or progression of one or
more disease processes.
One effort to make biomarkers more specific for cardiovascular
disease involves definition of a joint marker, such as C-reactive
protein and fibrinogen. Ranking in the highest quartile for both
markers identified 13% of study subjects compared with 25% with
use of only one marker. In addition, analysis showed that rank in
the highest quartile for both markers placed older people at 20-fold
short-term relative risk for infarction compared with the risk for
people placing in the lowest quartile for both.
|