|
|
| Cardiovascular
Complications of Diabetes Mellitus: East vs. West |

|
East:
Nobuhiro Yamada
University of Tsukuba
Tsukuba, Japan |

|
|
West:
Richard W. Nesto
Lahey Clinic Medical Center
Boston, MA, USA
|
|
|
East: Dr. Yamada opened with a historical
perspective of changes in lifestyle and in prevalence of diabetes
in Japan. The remainder of his talk focused on The Japan Diabetes
Complications Study, a large-scale, prospective study designed to
understand the epidemiology of diabetes and cardiovascular disease
in Japan better and to improve the medical management of adults
with type 2 diabetes.
West: Dr. Nesto used recently published material as a basis for
explaining why diabetic patients have a poorer outcome after acute
coronary events than patients without diabetes. He concluded by
presenting molecular targets for pharmacologic and other interventions
in the treatment of diabetic patients.
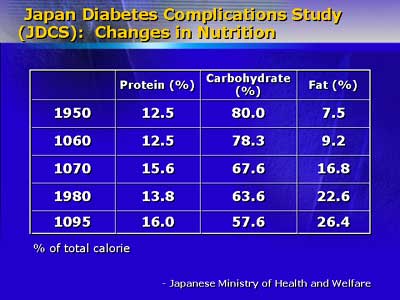
East: Dr. Yamada opened with a historical perspective of
changes in the past 50 years in Japan in lifestyle and in the prevalence
of diabetes mellitus. He noted significant changes in diet (increase
in fat from 7.5% to 26.4%, with drop in carbohydrates from 80.0%
to 57.6%) and daily activity, with a trend toward a more sedentary
lifestyle. During the same time frame, the prevalence of type 2
diabetes has increased more than 20-fold, to a prevalence of roughly
10% of adults over age 40 years.
|
 |
|
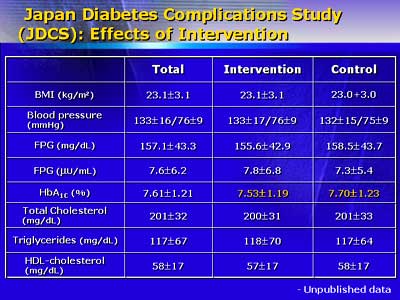
The Japan Diabetes Complications Study is the first large-scale,
prospective study to focus on the Japanese diabetic population:
It enrolled more than 2,000 patients previously diagnosed with type
2 disease and randomized them (in April 1996) to conventional care
or to intensive intervention. The groups are comparable in baseline
characteristics; he noted that their average body mass index of
23.1 is significantly lower than the average value in the West.
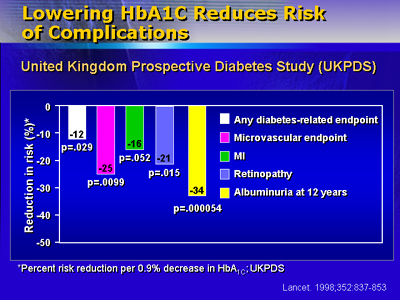
After 3 years, only one parameter, HbA1c level, has a statistically
significant difference, and that difference (7.70 for conventional
group versus 7.53 for the intervention group) is small.
|
 |
|
Acute coronary events and strokes are the macroangiopathic endpoints.
After 4 years, 44 patients had coronary events and 40 had strokes.
The frequencies of both are significantly higher than those for
non-diabetic Japanese adults. There was a gender differential for
heart disease (male greater than female), but none for stroke. Dr.
Yamada noted that frequencies of heart diseases are much lower than
those in the West. For instance, the incidence of coronary events
is less than one third of that cited in most Western studies. He
noted that a study of Hiroshima University showed that Japanese
living in Hawaii had coronary disease similar to that of Hawaiian
Caucasians rather than that of people living in Japan. He noted
that this supports the importance of environmental factors such
as nutrition in development and progression of atherosclerosis.
|
 |
|
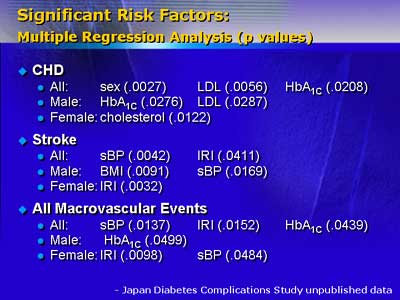
Analysis of the results from the first 4 years of endpoint data
show that the most important risk factors for coronary disease are
LDL cholesterol and HbA1c, with systolic blood pressure and fasting
insulin level most important for stroke. The study reviewers recommend
maintenance of LDL less than 140mg/dl, ideally less than 100mg/dl,
and maintenance of systolic pressure less than 150mm/Hg, and ideally
less than 130mm/Hg.
Dr. Yamada concluded with a re-emphasis on the difference in incidence
of coronary disease between Japanese and Western diabetics as evidence
that lifestyle, and thus lifestyle interventions, have direct impact
on atherosclerotic heart disease.
West: Dr. Nesto noted that many studies have found that
diabetic patients have poorer outcomes after acute coronary events
than patients without diabetes and that this phenomenon has triggered
an explosion in physician interest. The goal of his talk was to
present what is known about coronary disease in patients with diabetes
or impaired glucose tolerance and what avenues research is taking
to develop better medical care for this population.
The prevalence of diabetes in the United States has climbed from
4.7% in 1990 to greater than 6% in 1998, an increase of more than
60%. Thus, this population (as in Japan) is large and growing in
size.
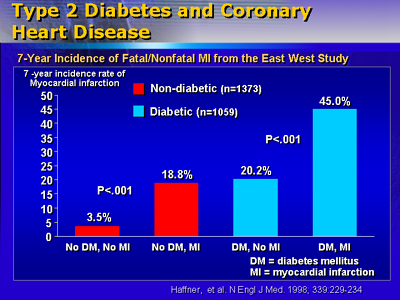
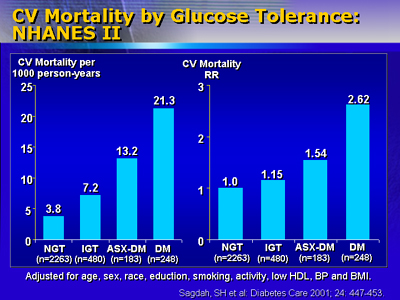
Dr. Nesto emphasized that recent studies have concluded that diabetes
is equivalent to coronary disease. One study showed that in 2 years
of follow-up, diabetic patients with a coronary event matched the
survival curve for non-diabetic persons who had a previous coronary
event. New, unpublished data from the GUSTO2B trial substantiates
that diabetic patients have poor outcomes that do not seem to depend
on factors seen in other patients. Prognosis for diabetic patients
was poor regardless of infarct size or whether the infarction showed
ST elevation or not. Patients who demonstrated impaired glucose
tolerance but were not diagnosed with diabetes had a prognosis similar
to that of patients with overt diabetes.
|
 |
|
Next, he discussed an autopsy series on more than 1,000 individuals
15-34 years of age with elevated HbA1c (8%) that was designed to
study the development and progression of atherosclerosis. Investigators
found that there was a significant prevalence of atherosclerosis
in this group. Roughly 45% of subjects had 5% or more of their right
coronary arteries covered in fatty streaks, and 16% had the same
extent covered with raised, atherosclerotic plaques. Clearly, atherosclerosis
begins and progresses years before diabetes is diagnosed.
|
 |
|
A recent study of angiographic results for diabetic patients shows
that this group tends to show a wide extent of atherosclerotic involvement
but with mild to moderate disease (with many lesions showing less
than 25% stenosis). The profile of extensive disease that does not
slowly progress to near complete occlusion places these people at
higher risk that a thrombotic or embolic event will precipitate
acute myocardial infarction.
Dr. Nesto then made the transition to discussion of what is physiologically
different in diabetic persons with atherosclerosis. For instance,
he cited studies indicating that C-reactive protein levels, a marker
for inflammation, are higher in people with type 2 diabetes of greater
than 10 years' duration. Elevated levels indicate a potentially
prothrombotic state and are a risk factor for both stroke and myocardial
infarction.
Another area in which diabetic patients are qualitatively different
lies in neuropathy. Investigators who conducted positron emission
scans of diabetic subjects and non-diabetic subjects with previous
myocardial infarction found that the pattern of autonomic neuropathy
shown by diabetic persons without a previous infarction was quite
close to that of non-diabetic patients with a previous myocardial
infarction.
Dr. Nesto stated that even after adjustment for all known risk
factors related to atherosclerosis, diabetic patients have a doubled
mortality rate after infarction compared with non-diabetic patients.
He hypothesized that prothrombotic states, autonomic neuropathy,
or both, along with as yet undefined physiologic differences, may
account for this difference in prognosis. As we learn more about
the physiology of persons with diabetes, we can develop appropriate
interventions.
|
 |
|
He concluded by noting that roughly 50% of patients without history
of diabetes who have presented to him in the cath lab have either
an impaired glucose tolerance or diagnostic diabetes when screening
is done. He reminded physicians to view coronary patients as possible
diabetic patients, too.
|
| Reporter: Elizabeth
Coolidge-Stolz, MD |
 |
copyright
 2001 by DOL Inc. All rights reserved..
2001 by DOL Inc. All rights reserved..
|
|
|