| Dr. Bashore noted
that most of the material on which he based his presentation is available
at the web site of the American College of Cardiology (www.acc.org).
He structured his talk to include guidelines for primary and rescue
percutaneous coronary interventions in the setting of acute infarction,
as well as discussion of prognostic interpretation of imaging results
and of catheterization as part of post-infarction risk stratification.
Dr. Bashore opened by noting that the relevant guidelines are available
at the web site of the American College of Cardiology (www.acc.org).
His first topic was the use of primary percutaneous intervention
as an alternative to thrombolytic therapy. The major indicators
include timing within 12 hours of symptom onset, persistent pain,
cardiogenic shock, or contraindication to thrombolytics.
Rescue interventions are generally done when there is less than
TIMI 2 flow rate in the infarct-related artery or there is evidence
of persistent ischemia or hemodynamic instability. He noted that
current guidelines do not recommend routine catheterization within
the first 48 hours after thrombolytic therapy.
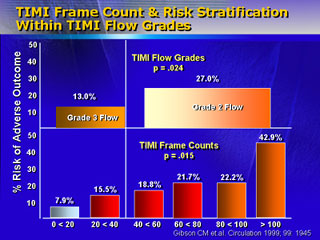
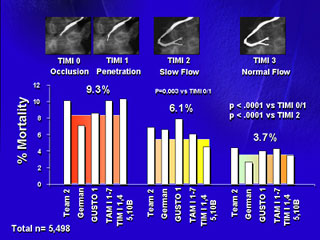
Dr. Bashore stated that much discussion about the prognostic value
of angiography is based on interpretation of findings. Perfusion
can be assessed by TIMI flow rates or frame counts. Counts represent
an attempt to standardize results into a simple index. The frame
count marks the time required for contrast to reach a preselected
landmark; it appears to have more prognostic power than flow rate.
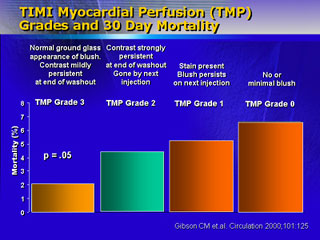
Another way in which prognostic information can be obtained involves
TIMI myoperfusion grades, which range from Grade 0 (no or minimal
blush) to Grade 3 (normal blush with persistent contrast to end
of washout). Intermediate grades reflect microvascular delay in
contrast washout.
High-risk patients should generally have catheterization as part
of risk stratification. He noted the following: patients older than
75 years, those in Killip class II-IV, patients with a non-ST-elevation
infarction or with new left bundle branch block, those with diabetes,
and those with cTroponin I levels greater than 1.5 ng/mL or with
a high BNP level.
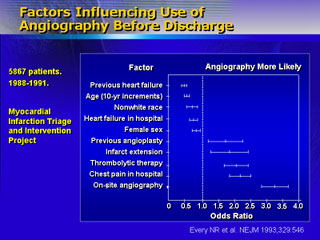
Dr. Bashore noted that the risk stratification guidelines encourage
physician flexibility. He drew attention to findings that indicate
certain populations, including women and elderly patients, are catheterized
less frequently than expected and reminded physicians to be aware
of those patients.
He concluded by noting that there is a clear trend toward an invasive
strategy emphasizing catheterization based on mortality-rate findings
from a number of studies published recently, especially in 2000
and 2001.
|