Chronic
resynchronization therapy plus an implantable defibrillator
reduces mortality by more than 40% in patients with moderate
to severe heart failure. This treatment approach also substantially
reduces hospitalizations attributable to heart failure. Resynchronization
therapy without the defibrillator had an effect on hospitalizations
but a less pronounced effect on mortality.
At a late breaking clinical trials session, Dr. Bristow
presented preliminary results of the COMParison
of MedicAl, ResynchronizatioN,
and DefibrillatION Therapies in Heart Failure
(COMPANION). The study evaluated chronic resynchronization
therapy, with or without an implantable defibrillator, in
patients with heart failure and QRS widening. The primary
hypothesis of this major clinical trial is that either therapy
would lower morbidity and mortality.
The study included patients with New York Heart Association
Class III or IV chronic heart failure and QRS width greater
than 130 milliseconds. To be eligible for the trial, patients
must have had a heart failure hospitalization within the past
12 months.
Investigators randomized the patients in a 1:2:2 fashion
into one of three groups. The first group received only optimal
pharmacological therapy for heart failure. The definition
of optimal pharmacological therapy was diuretics, beta blockade,
ACE inhibition or ARB substitution, spironolactone, and optionally,
digoxin. The second group received this optimal medical therapy
plus a biventricular cardiac resynchronization therapy device.
The third received optimal therapy plus a resynchronization
device and an implantable cardioverter defibrillator.
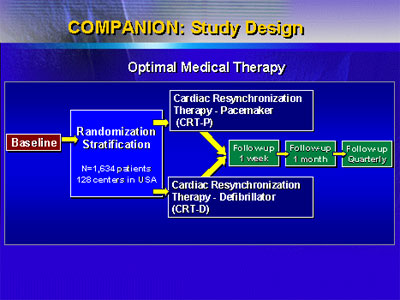
Dr. Bristow reported on 1,520 patients; 68% were men, the
mean age was 72 years, and 75% had Class III heart failure.
While more than 1,600 patients had enrolled, the trial met
its efficacy trial for termination in November 2002. Investigators
stopped tabulating efficacy endpoints soon after that.
The primary endpoint was time to all-cause mortality or
non-elective hospitalization. There was a significant reduction
in this endpoint for both the resynchronization group (18.6%,
p=0.015) and in the resynchronization plus defibrillator group
(19.2%, p=0.005).
Investigators found a highly significant reduction in mortality
in the group of patients that received both the resynchronization
device with defibrillator. There was a 43% reduction in mortality
rate at 12 months. There was a trend toward reduction in mortality
in the group of patients that received the resynchronization
device but no defibrillator. There was a 24% reduction in
mortality at 12 months.
Dr. Bristow and colleagues performed some further analysis
and found a 34% reduction in time to mortality or heart failure
hospitalization in the resynchronization group (p<0.001) and
a 38.3% reduction in the resynchronization/defibrillator group
(p<0.001).
While these are all preliminary data, the investigators
believe they accurately reflect what will be the ultimate
outcome of the trial.
One important question is whether either implantation strategy
will be cost effective. Investigators have not undertaken
economic studies yet. However, Dr. Bristow believes that both
approaches would be cost effective. This is because heart
failure hospitalizations are a major factor in the cost of
heart failure care. In the COMPANION trial, both approaches
provide a substantial reduction in heart failure hospitalizations.
A number of other recent trials have failed to show a benefit
of some intervention on top of optimal medical therapy. Now,
the COMPANION trial, plus the EPHESUS
trial Dr. Pitt presented here at ACC, show the opposite.
The results suggest that doctors can improve the outcomes
in heart failure beyond what they might expect to see with
today's standard medications.
|