| Depression
is very prevalent in patients with age-related macular degeneration.
Preliminary data suggests that teaching problem-solving skills
can help reduce depression and improve disability in patients
with this vision disorder.
In older adults, age-related macular degeneration
(AMD) is the most common cause of blindness. This disabling
vision disorder impairs the ability to complete many important
everyday tasks, such as housework, cooking, and travel.
Depression is common among individuals with AMD. According
to Dr. Rovner, the incidence of depression over 6 months is
28% among these individuals. Patients with AMD and depression
have higher levels of vision disability compared with non-depressed
AMD patients.
Because depression can compound AMD disability, Dr. Rovner
and colleagues have sought ways to reduce the burden of depression
in this patient population. Accordingly, they undertook a
randomized, controlled clinical trial of Problem-Solving Therapy
(PST).
The theory behind PST is that depression can stem from inaccurate
evaluation of problems, and difficulty finding solutions for
those problems. Teaching depressed individuals to think through
these problems and find solutions may ameliorate depression.
The study of PST included 118 older patients with AMD randomized
to PST or a control arm of usual care only. All patients were
over 65 and had AMD affecting both eyes. The AMD in the second
eye had to be of recent onset. Nurses visited the homes of
the subjects once weekly for 6 weeks to teach PST skills.
Investigators evaluated depression in patients at baseline,
2 months and 6 months.
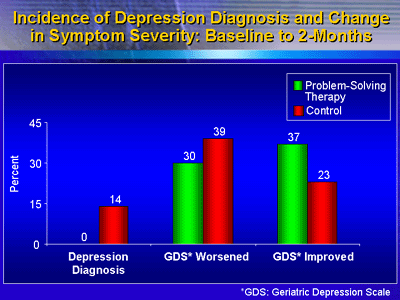
The study is still in progress. Here at IPA, Dr. Rovner presented
data from the 2-month evaluation. In the control group, 14%
had a diagnosis of depression at 2 months, versus no patients
in the group that received PST. Scores on the Geriatric Depression
Scale were more likely to improve in the PST group, and more
likely to worsen in the usual care group.
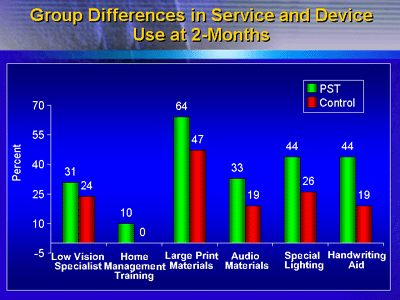
The PST therapy also improved vision function for activities
that AMD patients enjoyed, according to the investigators.
Patients in the PST group were less likely to discontinue
an activity due to poor vision function than controls (18%
versus 30%). In addition, patients in the PST group were more
likely to take advantage of large print materials, audio materials,
handwriting aids, and other services or devices.
These preliminary results suggest that PST prevents depression
and improves vision function for desired activities in AMD
patients. Dr. Rovner said that PST training is not expensive
but does require nurses conduct home visits. However, some
of this cost might be offset if patients are less likely to
become disabled, injured, or placed in a nursing home. If
final results of this and other studies are positive, then
psychogeriatrics experts might recommend PST as a routine
part of ophthalmologic care.
|