| Results
of this analysis suggest that sex differences may influence
brain structure and clinical features of late-life depression.
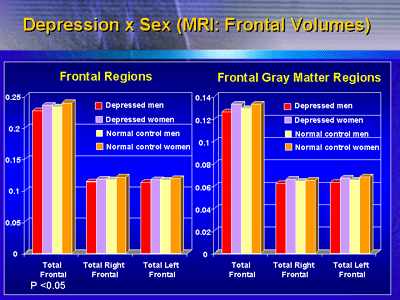
Men may be more susceptible to atrophy of frontal and gray matter
volume. This may promote vulnerability to depression. In elderly
women, hormone replacement therapy may improve apathy and mood,
but could reduce regional brain volumes.
Investigators have shown that in geriatric
depression, brain changes are associated with both vascular
disease and medical burden. In addition, an accumulating body
of research has evaluated the relationship between structural
brain changes with age, gender and comorbidity.
Some researchers have reported that older men exhibit increased
brain atrophy, placing them at increased risk of depression.
Changing hormones may affect brain atrophy as well. Some reports
suggest women on hormone replacement therapy (HRT) had more
brain atrophy than non-users.
To explore the interrelationship of brain structure and gender
in elderly depressed patients, Dr. Lavretsky and colleagues
compared patients with major depression and age-matched normal
controls. They evaluated regional brain volumes (total brain,
frontal and orbito-frontal gray and white matter) using magnetic
resonance imaging (MRI). They also assessed medical burden
and neuropsychiatric symptoms. In a subset of patients, they
explored the interrelationship of hormone replacement therapy
with MRI variables.
Investigators recruited 82 subjects 60 years of age or older,
including 41 with major depression (32 women) and 41 controls
(20 women). The mean age was 70.5 years in the cases and 72.2
years in controls. They measured depression and quality of
life using the short form-36 (SF-36) health questionnaire
and the Hamilton Depression Scale. They estimated medical
burden (vascular and non-vascular), psychomotor retardation,
apathy and cognition using appropriate scales.
The depressed subjects were more apathetic than controls
and had lower scores on the Mini-Mental State Exam. They also
had poorer-quality of life on SF-36 measures. They were also
more medically ill, but they did not have an increased number
of cardiovascular risk factors. Multivariate analysis of these
findings showed that men were more apathetic, more medically
ill and had more psychomotor impairment compared with women.
This was true for men in the depressed group and men in the
control group.
Dr. Lavretsky reported that brain volumes were smaller in
depressed men than in depressed women. Likewise, brain volume
was smaller in men in the control group versus female controls.
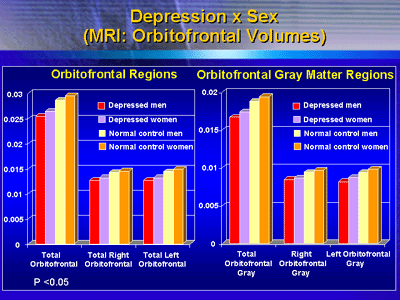
Investigators also compared orbitofrontal volumes in the
four groups. They found that depressed patients had lower
orbitofrontal volumes than controls. In addition, men had
lower orbitofrontal volumes than women in both the depressed
and control groups.
There were 16 women in the study taking HRT. This included
8 depressed women and 8 controls. They found the women taking
hormone replacement therapy were less apathetic. This was
particularly true for the cognitive part of the Apathy Evaluation
Scale (AES). This component of the AES evaluates interest
and motivation (i.e. “Getting together with friends is important
to her/him”). However, there was also evidence that women
on HRT had lower brain volumes compared with those subjects
not on HRT.
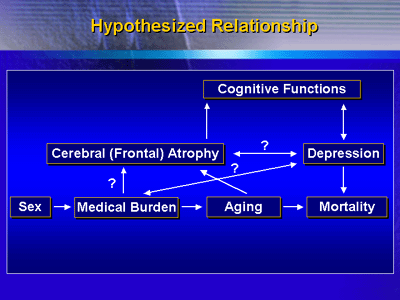
Based on these findings, Dr. Lavretsky and colleagues have
hypothesized a hierarchy of relationships between these variables.
The investigators will continue to evaluate gender differences
in geriatric depression. In particular, they will explore
the role of hormones in these complex relationships.
|