| A
wide range of epidemiologic and other studies indicate that
four risk factors for cardiovascular disease---hypertension,
abnormalities in glucose and insulin levels, cigarette smoking,
and obesity--- are also risk factors for vascular cognitive
impairment and dementia. Hypertension (particularly high systolic
blood pressure) appears to be the strongest predictor of significant
cognitive impairment in the elderly. Dr. Gorelick reviewed the
literature and explained a possible mechanism for cerebral neurotoxicity
through primary disruption of endothelium in the brain’s blood
vessels. As a conclusion, he stressed the importance of diagnosing
and treating hypertension. Aggressive midlife medical care for
cardiovascular disease may have significant benefits in decreasing
the risk for late-life vascular cognitive impairment and dementia.
Dr. Gorelick opened by noting that studies
have suggested certain genetic and clinical characteristics
are associated with healthy aging. For instance, there may
be roughly 1000 genes associated with longevity, with at least
one major gene localized to chromosome 4. There are multiple
clinical characteristics shared by those who live long and
in good health. Four such traits are low blood pressure, low
serum glucose, no cigarette smoking, and no obesity.
When viewed differently, it is clear that risk factors for
cardiovascular disease --- hypertension, abnormal glucose
and insulin levels, cigarette smoking, and obesity --- are
also risk factors for cognitive health in late life. Based
on data from numerous studies, hypertension, especially elevated
systolic blood pressure, appears to be the strongest predictor
of vascular cognitive impairment and dementia among the elderly.
Older research uses the model of vascular dementia to understand
pathologic cognitive declines. Imaging and etiologic studies
of patients with vascular dementia identify subtypes such
as multi-infarct dementia, as well as dementia associated
with a strategically important infarct (often involving the
angular gyrus or thalamus) or dementia associated with diffuse
subcortical damage.
Over time, the model has shifted to one of vascular cognitive
impairment characterized by a combination of etiologic and
clinical traits. Vascular cognitive impairment is actually
a spectrum of syndromes that have decreased cognitive ability
across multiple domains at their centers. Impairment can range
from slight to severe, and the time course ranges from sudden
to subacute to slow development and progression.
Multiple direct causes have been identified, including clinical
and silent strokes. Pathologic findings include microvascular
disease, large-artery disease, deposition of A-beta peptide,
or cerebral hemorrhage. Vascular cognitive impairment embraces
a variety of heterogeneous syndromes, and distinction from
Alzheimer’s dementia and direct stroke effect, both common
in the elderly, complicates the research and clinical picture.
Gorelick restated the research and clinical problem from
the public health perspective: ‘Can you identify early-phase
vascular cognitive impairment and intervene to prevent dementia?’
He believes the answer is ‘Yes.’ He noted epidemiologic studies
suggesting that roughly half of people with cognitive impairment
but no dementia develop dementia in five years, which suggests
there may be a target for preventive intervention. A twin
study showed that the twin with higher midlife systolic blood
pressure, metabolic abnormalities involving glucose and/or
insulin levels, or both was at higher risk for late-life dementia.
|
Population Attributable
Risk (PAR)
of Select Modifiable Stroke Risk Factors
for Vascular Cognitive Impairment
Factor
|
Relative
Risk |
Prevalence |
PAR |
| Hypertension |
8.7 |
25% |
66% |
| Diabetes mellitus |
1.8 |
10% |
8% |
| LDL-cholesterol |
2.6 |
36% |
37% |
| Atrial fibrillation |
1.5 |
4% |
2% |
| Current cigarette smoker |
1.8 |
25% |
17% |
Alcohol:
2-5 drinks/day |
1.8 |
7% |
5% |
Source: Gorelick P, 2003
|
He moved from an understanding of vascular cognitive impairment
and dementia and their risk factors to study of possible mechanisms
through which risk factors might contribute to clinically
evident cognitive decline.
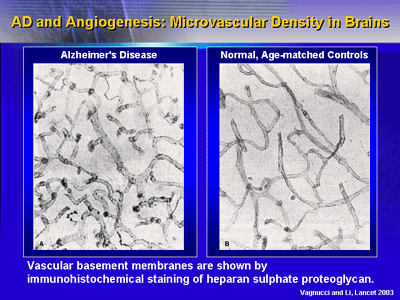
He presented findings from a 2003 paper on Alzheimer’s disease
and microvascular angiogenesis to frame the hypothesis that
cerebrovascular damage (specifically, disruption of the endothelium
and its action as a blood-brain barrier) can lead to neurotoxic
effects through a combination of soluble factors and deposition
of beta-amyloid protein.
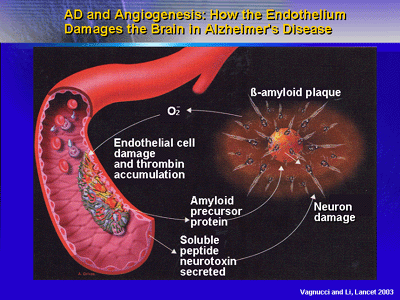
Neurotoxicity may be evident clinically as Alzheimer’s disease
or as vascular cognitive impairment or nonAlzheimer’s dementia.
Gorelick placed studies that did not find a link between
risk factors, especially hypertension, and cerebrovascular
disease and dementia in context by emphasizing that blood
pressure is known to decrease as cognitive impairment worsens.
He believes some studies may have missed a link between hypertension
and vascular cognitive impairment by evaluating people too
late in the course of their clinical presentation.
Gorelick concluded that research work as varied as epidemiologic
studies on healthy aging to anatomic and molecular work on
dementia lead to the same conclusion: Control of vascular
risk factors by midlife can decrease the risk for vascular
cognitive impairment and dementia at the end of the lifespan.
Hypertension is probably the most important target for such
intervention.
|