|
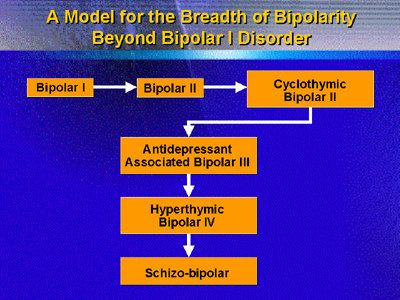
Dr. Akiskal answered the key question
of the symposium (Is there a bipolar spectrum?) with one word:
Yes. He discussed previous literature identifying a broad bipolar
spectrum; explained the clinical importance of identifying and
treating patients with different forms of Bipolar II disorder
(which, he believes, may comprise a spectrum of disorders);
and reviewed recent genetic linkage studies suggesting that
a similar genotype underlies some forms of schizophrenia and
Bipolar II disorder.
Dr. Akiskal opened by noting that the concept of depression
associated with hypomania or mania is very old in the medical
literature. Kraepelin formulated the modern model of manic-depressive
illness including recurrent depressive episodes. Conceptualization
of mood disorders has broadened from this paradigm (now diagnosed
as Bipolar I) as the last several decades of research have
shown that bipolar I patients often present with psychotic
symptoms.
Dr. Akiskal asserts that much of the bipolar spectrum relates
to Bipolar II (rather than Bipolar I, which is relatively
uncommon). He believes that the key clinical question is to
define the presentations and psychopathology that mark the
breadth of the spectrum so that research can lead to better
understanding and treatment.
He feels it is important to identify patients falling into
the spectrum of Bipolar II illness for several reasons: First,
the prevalence of such illness may be very high, up to 25%;
second, identification permits appropriate treatment with
mood stabilizers rather than inappropriate treatment with
antidepressants for a presumptive depressive illness. (He
cited one case in which a patient who felt depressed improved
somewhat when treated with antidepressant medication, but
then became uncomfortable and reported feeling "excited."
The patient experienced long-term improvement when treated
with a mood stabilizer.) Finally, inaccurate diagnosis and
inappropriate treatment may be associated with a high suicide
rate.
He noted several clinical clues that may help identify patients
with bipolar II spectrum illness.
Characteristics common to Bipolar II spectrum illness
・ |
Strong family history, including basic temperament
and presence of panic or other non-mood disorder
| ・ | Early
age at onset or postpartum onset in women | ・ | Personal
history characterized by mood cycling, mixed
states, or two or more days of hypomania during
depressive episodes. |
|
|
Dr. Akiskal recommends that any patient who has failed treatment
for depression three times, particularly if he or she shows
any of the clues, be considered for a diagnosis of Bipolar
II spectrum illness and treated accordingly.
Beyond clinical evidence lies research, and Dr. Akiskal
noted a number of recent genetic linkage studies that suggest
an association between genes correlated with schizophrenia
and genes correlated with Bipolar disorder, especially Bipolar
II.
He summarized his overall impression of the bipolar spectrum
as an activation disorder marked by dysregulation of affect,
as well as the possible presence of elements of phobia, anxiety,
panic, and psychosis.
|