|
Depression in schizophrenia is hard to
diagnose and treat. A method for obtaining an accurate diagnosis
of depression in schizophrenia was discussed. Strategies for
treating depression in schizophrenic patients were presented.
Dr. Siris noted that depression in schizophrenia is associated
with patient and family suffering and suicidal behavior. This
is an important because approximately 10% of all schizophrenic
lives end in suicide.
In order to diagnose depression in schizophrenic patients,
the physician must first eliminate all other possible disorders.
Many disorders mimic depression such as anemia, cancer, pulmonary
disorders, autoimmune disorders and endocrine disorders. To
establish the differential diagnosis of depression, the following
factors should be taken into account: comorbid medical conditions;
neuroleptic side effects such as akinesia, akathisia, dysphoric
or anhedonic reactions; acute or chronic use and/or discontinuation
of substances including "street" drugs, alcohol, nicotine
and caffeine. Other factors to be considered are acute and
chronic disappointment reactions; the "negative symptom" syndrome
and demoralization syndrome. The clinician should realize
that depression may be an intrinsic component of decompensation,
either on a biological or psychological basis or may result
from a psychotic episode. It is also possible that the patient
may have an independent coexisting affective diathesis or
schizoaffective disorder.
Once diagnosed, depression in schizophrenic patients may
be treated in a number of ways. The first strategies to consider
are to reduce or adjust neuroleptic dosage and change antipsychotic
agents to "atypical" antipsychotics. Alternate strategies
are the use of adjunctive agents such as antiparkinsonian
agents or tricyclic-type antidepressants. Depending on the
response obtained, non-tricyclic-type antidepressants such
as selective serotonin reuptake inhibitors (SSRIs), monoamine
oxidase inhibitors (MAOIs), benzodiazepines, propranolol and
electroconvulsive therapy may be used. Lithium and anticonvulsant
agents can also be used. These medications may be used alone
or in conjunction with psychosocial approaches.
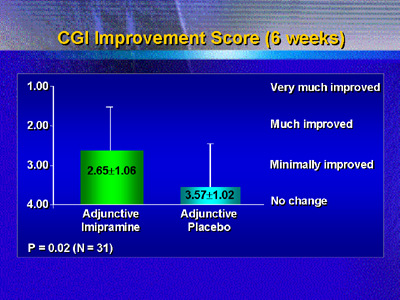
Dr. Siris noted that his first therapeutic decisions are
to either lower the dose of neuroleptics, change to an atypical
antipsychotic agent or use an adjunctive tricyclic antidepressant
such as imipramine. After 6 weeks on adjunctive imipramine,
patients reported significant (P < 0.02) improvements in their
clinical global impression (CGI) scores. Patients receiving
a adjunctive placebo reported little to no change in their
CGI scores.
|