|
Dr. Fischbach, a distinguished neuroscientist
who has served at universities and the National Institutes of
Health, addressed the progression of neuroscientific understanding
from the basic research findings of the 20th Century
to the current possibilities inherent in the integration of
neuroscience with clinical medical work. He used neurodegenerative
disorders, including Parkinson's disease and schizophrenia,
to illustrate many points.
Dr. Fischbach opened by noting that he would be addressing
three major groups in 2002−the American Psychiatric Association,
the American Neurological Association, and the American Neurosurgical
Association−and that this breadth of audience reflects the
growing understanding within different medical specialties
that much of the basic science underlying different clinical
developments is the same.
He noted that Sigmund Freud moved from electrophysiologic
work to psychological conceptualization because he needed
to seat his results within a theory of mental life. In contrast,
current scientists will use improved understanding of psychopathology
and psychopharmacology to revolutionize theories of cognitive
understanding and mental life.
Dr. Fischbach laid the groundwork for the remainder of his
talk in a discussion of the diversity of known neurodegenerations
(see Table), all of which at some level raise the question
of how to activate and deactivate apoptotic neuronal loss.
|
A sampling of neurodegenerations
at different stages of life.
| Disorders of the aging brain: Alzheimer's
disease, Parkinson's disease | | Disorders of younger adults: Huntington's
disease, amyotrophic lateral sclerosis, prion diseases | | Disorders
of children: spinocerebellar ataxia, Tay-Sachs
disease and other storage diseases |
|
|
He laid out a general framework that may apply to many of
these seemingly diverse conditions:
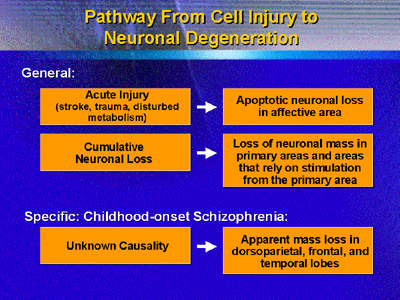
Dr. Fischbach noted that the mass loss with schizophrenia
can be quite large, in the magnitude of 2-3% loss per year,
especially in the dorsoparietal cortex. With this knowledge,
he believes researchers can find clues to the region of the
brain within which the disordered thought of schizophrenia
begins (the dorsoparietal cortex). When region can be confirmed,
studies to arrest or reverse neuronal loss in the target region
may begin.
This transition from understanding of key areas to work
in arresting or reversing neurodegeneration has already occurred
with Parkinson's disease, where he noted the success of pilot
studies that targeted regions within the subthalamic nucleus
for deep-brain stimulation.
In one case, functional magnetic resonance during electrode
placement allowed researchers to place an electrode so precisely
that the patient's contralateral motor symptoms were extinguished.
Initial results from some studies suggest that long-term stimulation
may even have trophic effects.
In summary, he believes it likely that much of the current
functional and imaging work done with psychiatric conditions
will reveal key locations of neuronal dysfunction and loss.
Once target locations are established, further work may reveal
the mechanisms through which loss occurs and the means through
which loss can be arrested or reversed.
He closed with an observation drawn from work with Parkinson's
disease: When the earliest clinical signs are seen, roughly
75% of neurons in the target region have already been lost.
Thus, early diagnosis of individuals at risk for disease or
presenting with early-stage disease is critical to improved
care and better prognosis.
|