| In patients
with complicated acute myocardial infarction, baseline levels
of B-type natriuretic peptide (BNP) and N-terminal BNP (N-BNP)
appear to strongly predict adverse mortality and unplanned rehospitalization.
Change in N-BNP over the month following acute myocardial infarction
also seems highly predictive of adverse outcomes. None of these
peptides predicted reinfarction.
Natriuretic peptide levels in plasma can provide
clinically relevant information on prognosis and left ventricular
function following acute myocardial infarction. Researchers
have investigated a number of natriuretic peptides. However,
there have been few direct comparisons showing the relative
prognostic value of these entities.
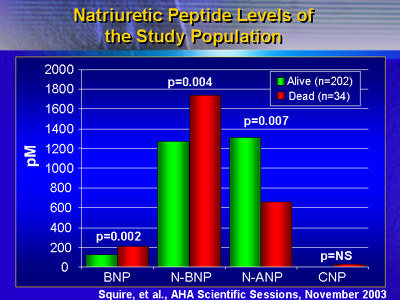
Dr. Squire and colleagues have completed a comparison of
B-type natriuretic peptide (BNP), N-terminal BNP (N-BNP),
N-terminal atrial natriuretic peptide (N-ANP) and C-type natriuretic
peptide (CNP). The comparison shows the value of these 4 different
natriuretic peptides in predicting death, reinfarction and
hospitalization after complicated acute myocardial infarction.
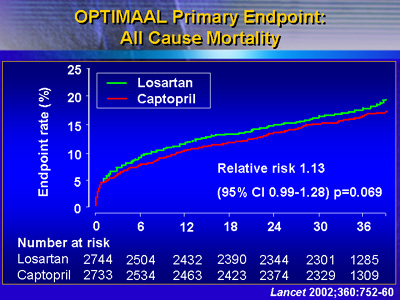
The analysis is part of a neurohormonal substudy of OPTIMAAL
(Optimal Trial in Myocardial Infarction with the Angiotensin
II Antagonist Losartan). The main purpose of the trial was
to compare losartan to captopril in patients with heart failure
or left ventricular dysfunction following acute myocardial
infarction.
In the neurohormonal substudy, investigators acquired natriuretic
peptide levels for 236 patients. This included 121 patients
who received losartan and 115 on captopril. They took measurements
at randomization, then at one month, 1 year and 2 years after
myocardial infarction.
The mean follow-up was 958 days. There were 14 deaths in
the first 30 days following myocardial infarction. An additional
20 deaths occurred after 30 days. There were 40 reinfarctions
and 134 hospitalizations.
Temporal Release of Peptides
Investigators found very different patterns of secretion
of these 4 peptides after myocardial infarction. This implies
that natriuretic peptides are not a homogeneous group of compounds
subject to the same stimulus.
Both BNP and N-BNP levels were high within a few days of
acute myocardial infarction. There was a steady drop-off at
1 month and 1 year.
Levels of N-ANP exhibited a different pattern. Circulating
levels increased significantly between baseline and 1 month.
Levels fell somewhat between 1 month and 1 year, but in the
following year, there was a significant decrease.
By contrast, CNP levels remained steady between baseline
and one month, then fell significantly over 1 year, and increased
slightly at the year 2 measurement.
Mortality
Baseline BNP and N-BNP were strong predictors of mortality
at 30 days, with p values of 0.001 and 0.004, respectively,
according to Dr. Squire. Baseline N-ANP levels were also predictive
(p = 0.012), but baseline CNP levels were not. The only baseline
measurement that predicted mortality after 30 days was N-BNP
(p = 0.05).
Reinfarction
None of the peptides predicted reinfarction over the follow-up
period.
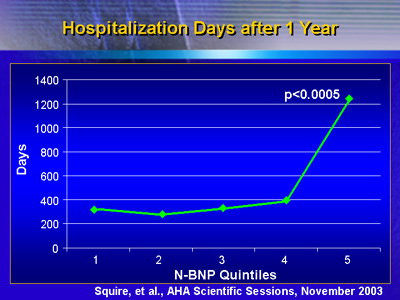
Hospitalization During Follow-up
Peptide levels at baseline and 1 month did not predict later
hospital days. However, N-BNP level at 1 year was a powerful
predictor of the number of hospital days (p < 0.0005).
In addition, the mean number of hospital days was higher
among patients who had higher than median levels of N-BNP
or N-ANP. However, these findings did not reach statistical
significance.
Treatment Outcomes
The change in N-BNP between baseline and 1 month was highly
predictive of outcome, according to Dr. Squire. In patients
who had positive outcomes past 1 month, n-BNP fell significantly
more than for patients who had adverse outcomes thereafter.
According to Dr. Squire, this finding indirectly supports
work from Japanese investigators indicating that n-BNP may
be a marker for efficacy of therapy in heart failure.
Together, these results suggest that baseline levels of BNP
and n-BNP strongly predict mortality and unplanned rehospitalization
in patients with complicated acute myocardial infarction.
Change in N-BNP between baseline and 1 month is also highly
predictive of adverse outcomes; in particular, patients with
less change over time have worse outcomes.
Both BNP and N-BNP appear to be consistent and powerful predictors
of outcomes for patients who have an acute myocardial infarction
with evidence of heart failure or left ventricular dysfunction.
Measuring plasma levels of these peptides may help further
substratify patients into high risk and very-high-risk groups.
One day, physicians may use BNP or N-BNP to identify patients
who require more intensive or aggressive therapy.
|