|
The beta-blocker atenolol reduced hyperemic myocardial perfusion,
while perindopril did not. Thus, beta-blocker therapy appears
to attenuate myocardial vasodilatory capacity compared with
angiotensin-converting enzyme (ACE) inhibition. This suggests
ACE inhibitors and beta-blockers have differential effects on
myocardial circulation. The differential effect occurs despite
the fact that these treatments reduce blood pressure to a similar
degree. Changes in myocardial microcirculation
are a characteristic feature of essential hypertension. Research
has shown that in hypertensive patients, the myocardium has
decreased perfusion reserve and increased minimal vascular
resistance. These abnormalities may relate to changes, such
as narrowing, in resistance artery structure.
Previous investigations have shown that angiotensin-converting
enzyme (ACE) inhibitor treatment improved resistance artery
structure. By contrast, beta-blocker treatment did not improve
resistance artery structure, even though it reduced blood
pressure to a similar degree.
Based on those findings, Dr. Buus and co-investigators hypothesized
that an ACE inhibition would also improve minimal myocardial
vascular resistance, while beta-blockade would not. To test
this, they compared long-term treatment with the ACE inhibitor
perindopril or the beta-blocker atenolol in patients with
essential hypertension. They evaluated the effect of treatment
on myocardial perfusion and vascular resistance.
The researchers randomized 30 patients (mean age 50 years)
with previously untreated essential hypertension to perindopril
(4-8 mg) or atenolol (50-100 mg). Researchers allowed dosage
adjustment to reach a diastolic blood pressure of less than
90 mmHg. They measured myocardial perfusion at rest and during
dipyridamole-induced hyperemia using positron emission tomography.
These measurements occurred before and after 12 months of
treatment.
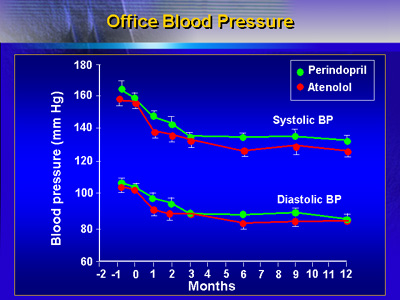
Reduction in blood pressure was similar between the two treatment
groups. Ambulatory blood pressure decreased in the perindopril
group from 160/105 to 138/88 mmHg (p < 0.01). Blood pressure
reduction decreased from 158/105 to 131/86 mmHg in the atenolol
group (p < 0.01).
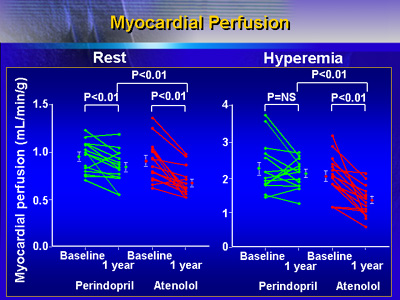
Both drugs decreased resting myocardial perfusion. In the
atenolol group, the decrease was from 0.91 to 0.67 ml/g/min.
There was a smaller decrease in the perindopril group, from
0.95 to 0.84 ml/g/min. However, there was no difference between
treatments when investigators corrected for changes in myocardial
workload (expressed as the rate-pressure product). On the
other hand, atenolol markedly reduced hyperemic myocardial
perfusion, while perindopril did not.
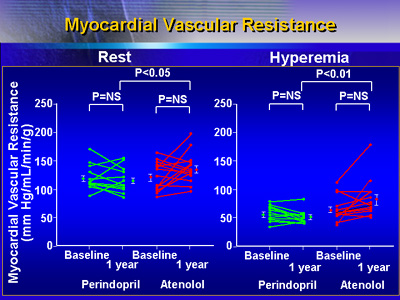
In addition, atenolol significantly increased hyperemic vascular
resistance compared with perindopril.
These results suggest that there is a difference in the way
ACE inhibition and beta-blockade affect myocardial circulation.
This difference occurs despite similar reduction in blood
pressure. Both drugs reduce resting myocardial perfusion.
However, atenolol markedly reduces hyperemic myocardial perfusion,
while perindopril does not. Atenolol increases hyperemic vascular
resistance compared with perindopril.
Based on these results, it appears that patients may require
a vasodilating therapy to improve hypertensive myocardial
microcirculation. |