| This pharmacokinetic
study shows that the beta-blocking effect of carvedilol continues
long after its elimination from plasma. Even after withdrawal
of medication, the beta-blocking effect remains for at least
44 hours. This may occur because the receptor binding of carvedilol
is persistent and nearly irreversible.
Treatment with beta-blockers such as carvedilol,
metoprolol and bisoprolol significantly reduces mortality
in patients with congestive heart failure. Results of the
Carvedilol or Metoprolol European Trial (COMET) showed that
carvedilol was superior to metoprolol. For example, investigators
found a significantly greater risk reduction in cardiovascular
mortality versus metoprolol (20% risk reduction) and death
due to stroke (67% risk reduction).
One possible reason for this advantage is that carvedilol
blocks multiple adrenoreceptors. In contrast, metoprolol is
selective for the beta-1 adrenoreceptor. Others have suggested
that carvedilol has ancillary properties, such as an antioxidant
effect.
Another possible explanation is that carvedilol has atypical
binding kinetics. Researchers have reported that the binding
of this beta-blocker to myocardial membranes is nearly irreversible.
This raises the possibility that the beta-blocking effect
of carvedilol may persist even after plasma elimination.
To test this hypothesis, Dr. Kindermann and colleagues compared
catecholamine response in the heart during carvedilol or metoprolol
administration, and after abrupt withdrawal of either beta-blocker.
They performed in vitro investigations on isolated and electrically
stimulated human atrial muscle strips. They also performed
in vivo experiments in 7 healthy volunteers.
In Vitro Experiments
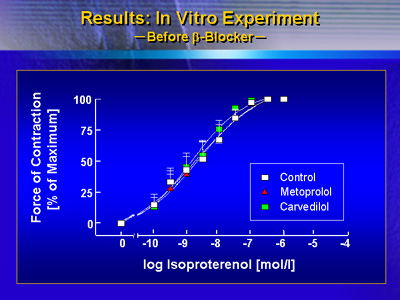
Investigators measured the contractility of isolated, electrically
stimulated human atrial muscle strips in response to isoproterenol.
They measured contractility before applying beta-blockers,
during incubation with beta-blockers, and after withdrawal.
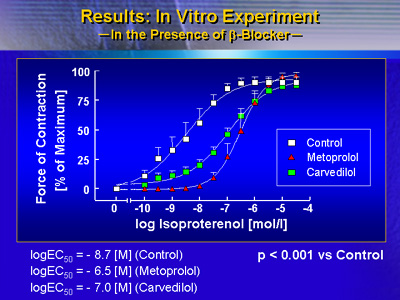
During beta-blocker application, there was significant reduction
in the potency of isoproterenol compared with control conditions.
This occurred for both carvedilol and metoprolol.
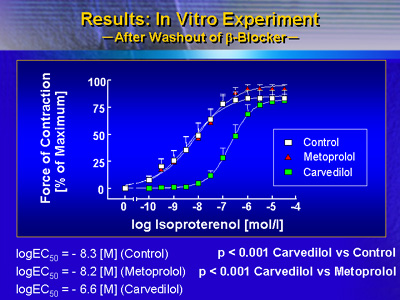
However, there was a striking difference between beta-blockers
when investigators removed atrial muscle strips from the beta-blocker
solution. After washout of beta-blockers, isoproterenol potency
returned to baseline levels for metoprolol. In contrast, the
potency of isoproterenol remained lower. This difference was
highly significant, Dr. Kindermann said.
In Vivo Experiments
Seven healthy volunteers received 50 mg of carvedilol and
190 mg of metoprolol for 10 days in a randomized, crossover
study. They all underwent dobutamine stress echocardiography
before, during and 44 hours after receiving study medication.
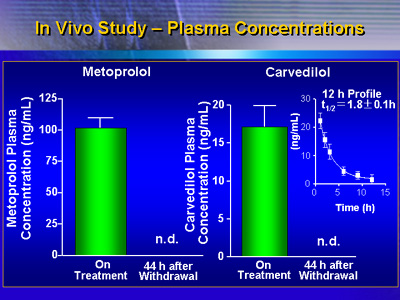
Plasma concentrations of carvedilol and metoprolol during
treatment were within the therapeutic range; at the 44-hour
measurement, plasma concentrations were below detectable levels
in both groups.
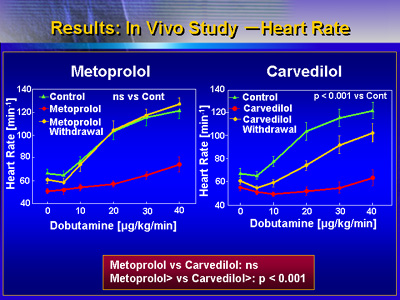
Heart rate response during therapy was comparable between
beta-blockers. Both metoprolol and carvedilol resulted in
a significant reduction of heart rate response during dobutamine
stimulation in all volunteers. However, after withdrawal of
medication, the heart rate response returned to baseline levels
for metoprolol. On the other hand, there was still a beta-blocking
effect for carvedilol.
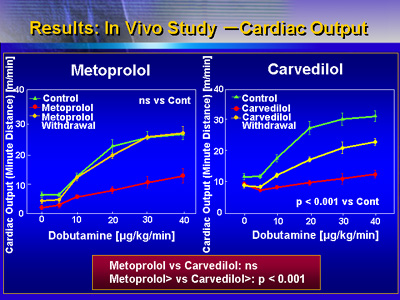
Similarly, cardiac output in response to dobutamine was different
between beta-blockers. Cardiac output returned to baseline
levels 44 hours after withdrawal of metoprolol. In contrast,
cardiac output remained depressed after withdrawal of carvedilol.
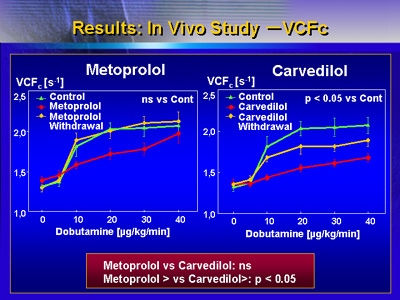
Investigators made similar observations for heart rate-corrected
velocity of circumferential fiber shortening (VCFc). After
withdrawal of metoprolol, this parameter returned to baseline
values, whereas it remained significantly reduced in carvedilol-treated
volunteers.
These results show that the beta-blocking effect of carvedilol
continues long after its selimination from plasma. This may
occur because of persistent receptor binding.
These findings show that carvedilol prevents a beta-blocker
rebound phenomenon. Even after withdrawal of medication, the
beta-blocking effect remains for at least 44 hours. Compliance
to carvedilol therapy may not be as critical as in other beta-blocker
therapy. The beta-blocking effect may remain even if patients
occasionally miss a dose.
|