|
Carvedilol, in addition to an angiotensin-converting
enzyme (ACE) inhibitor, has a favorable influence on remodeling
in patients who have left ventricular dysfunction after an acute
myocardial infarction. Investigators reported improvements in
left ventricular end-systolic volume, left ventricular end-diastolic
volume, left ventricular ejection fraction and wall motion score
index. Early treatment benefits appear to come from both the
beta blocking and vasodilatory effects of carvedilol. Later
in treatment, the vasodilatory effect attenuates, and the benefit
derives mainly from beta blockade.
Convincing data suggests that angiotensin-converting enzyme
(ACE) inhibitors improve left ventricular remodeling in chronic
heart failure, and in patients with left ventricular dysfunction
after myocardial infarction.
Carvedilol also improves remodeling in heart failure patients.
There is data showing that carvedilol improves remodeling
in heart failure and after myocardial infarction. However,
the post-myocardial infarction data comes from a study of
carvedilol without ACE inhibitor. There was no data showing
the effects of carvedilol plus ACE inhibitor on ventricular
remodeling.
Investigators initiated a study to fill this data gap. This
was a substudy of the CAPRICORN (Carvedilol Post-Infarct Survival
Control in Left Ventricular Dysfunction) trial. The purpose
of this study was to show the change in end-systolic volume
in post-myocardial infarction patients who received carvedilol
plus ACE inhibitor. The researchers used quantitative two
dimensional echocardiography at baseline, 1, 3 and 6 months.
The substudy included 58 patients who received carvedilol
and 67 who received placebo. In contrast to previous remodeling
studies of post-myocardial infarction patients, a significant
number of patients had prior history of myocardial infarction
or heart failure (about 25% and 42%, respectively).
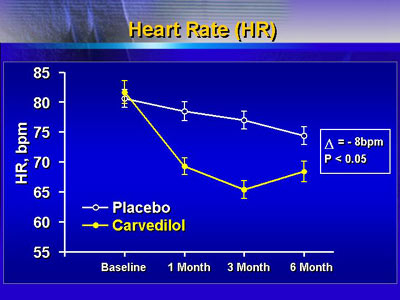
Carvedilol plus ACE inhibitor significantly reduced heart
rate. At the end of 1 month, there was a marked reduction
of about 8 beats per minute vs. placebo. At 3 months, the
reduction was 12 beats per minute. This effect attenuated
somewhat by month 6, for an overall reduction of 8 beats per
minute.
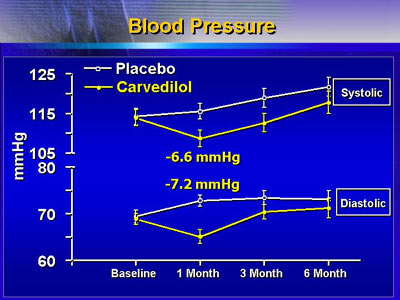
There was a profound reduction in systolic and diastolic
blood pressure at 1 month. There was also a reduction of blood
pressure vs. placebo at 1 month (6.6 mmHg difference in systolic
and 7.2 mmHg diastolic). By 3 months, the effect continued
for systolic blood pressure, while diastolic blood pressure
was similar for carvedilol and placebo.
Carvedilol plus ACE inhibitor also decreased left ventricular
end-systolic volume at 1 month. There was an early increase
in the placebo group, and an early decrease in the carvedilol
group. These effects continued out to 6 months, with perhaps
a slight further reduction with carvedilol. Overall, there
was an 11% reduction in this measure at 6 months (p=0.037).
In addition, carvedilol plus ACE inhibitor somewhat attenuated
increase in left ventricular end-diastolic volume. At 6 months,
the difference was about 5%, or approximately 7 ml lower in
the carvedilol group.
There was an early improvement in stroke volume at 1 month.
This continued to 3 months. Because of a progressive increase
in the placebo group, there was not a statistically significant
difference in stroke volume at 6 months (p=0.053).
Likewise, left ventricular ejection fraction improved early
and continued throughout the course of treatment. Overall,
there was an absolute improvement in ejection fraction of
4 percentage points vs. placebo (p=0.0037). There was also
early reduction in wall motion. This improvement attenuated
over time and was not statistically different at 6 months.
This study suggests carvedilol provides different benefits
to patients, depending on the length of treatment time.
The early and sometimes dramatic improvements in heart rate,
blood pressure, stroke volume, left ventricular ejection fraction
and left ventricular end-systolic volume are consistent with
both the beta blocking and vasodilating effects of carvedilol.
The vasodilating effects appear to attenuate with time,
as shown by the reduction in effect on heart rate, blood pressure
and stroke volume. This is also when the improvement in left
ventricular end-systolic volume is most obvious, showing the
beta blocking benefit of carvedilol.
|