|
Depression is strongly associated with
a worse prognosis in patients with established coronary artery
disease. Despite the evidence, there have only been two trials
of depression treatment in this patient population. Physicians
need to consider depression as a risk factor in patients with
established coronary artery disease and treat it when appropriate.
More treatment trials should be conducted.
Depression is a potential new risk factor for coronary artery
disease (CAD), similar to obesity and lack of exercise. There
is emerging evidence to suggest that although depression may
not cause CAD, treating depression would be prudent in such
patients.
The prevalence of major depression is high in hospitalized
CAD patients. There is good data to suggest that major depression
is at least 3 times as common in these patients as in the
general community for hospitalized patients. This is true
in a variety of populations, including myocardial infarction,
unstable angina, congestive heart failure and post-intervention
patients.
Interestingly, minor depression is also about 3 times as
common in hospitalized CAD patients. This means that about
one third of these patients show some degree of depression
during hospitalization.
It is difficult to predict which CAD patients will exhibit
depression. However, it is more common in women, younger patients,
individuals with poor social support and patients with more
severe CAD.
Researchers do not know exactly what causes depression.
It is likely that a combination of genetics, unhealthy lifestyles
and previous stresses create physiologic susceptibility. Then,
stressful life events or chronic stress can interact with
this susceptibility. This causes neuroendocrine disturbances
that result in depression.
It is possible that there is a link between the causes of
depression and CAD. There is no causal link. However, the
neuroendocrine disturbances of depression may have an impact
on the platelet changes, inflammation and autonomic nervous
system disturbances that contribute to atherosclerosis.
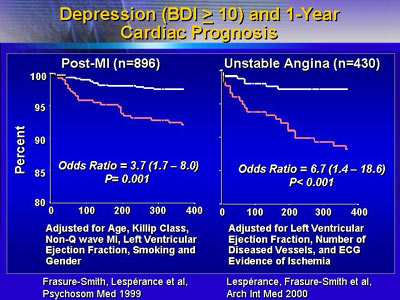
Dr. Frasure-Smith and colleagues have studied the psychosocial
aspects of acute coronary syndromes. They have looked at 896
post-myocardial infarction patients and 430 patients with
unstable angina who all received usual care (31% women).
The investigators found that depression had a marked impact
on 1-year prognosis, even after adjusting for other major
cardiac risks. The impact was most pronounced in the first
6 months, then decreased somewhat.
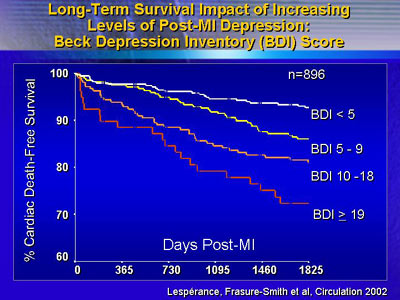
They also found a dose-response relationship. Patients with
worse depression had a worse prognosis. This suggests there
may be no safe level of depressive symptoms for CAD.
This is not the only study to suggest a dose-response relationship
between depression and CAD outcomes. A 1996 study in the American
Journal of Cardiology looked at depression severity in 1,250
catheterization patients. More deaths occurred in patients
with moderate/severe depression compared with patients who
had mild depression. Adjusting for other cardiac risks, the
investigators found that long-term risk of mortality was significantly
higher in patients who were depressed.
Consistent results emerged from a more recent study of older
patients. A 2001 study in the Archives of General Psychiatry
looked at patients age 55 to 85 years with a history of angina,
myocardial infarction or congestive heart failure.
There are no prospective studies yet to demonstrate whether
treating depression can alter CAD prognosis. However, Dr.
Frasure-Smith believes that there is enough evidence to justify
additional trials. That evidence should compel physicians
to consider depression as a risk factor in patients with established
CAD.
|