|
Important risk factors for stroke in
Western countries include hypertension, diabetes, smoking, and
atrial fibrillation. Western researchers are increasingly using
subclinical disease markers to risk stratify patients. There
are a number of important differences in stroke epidemiology
between East and West. However, there are more similarities
than differences. Both Western and Eastern countries underutilize
risk factor modifications such as smoking cessation.
In the United States, there are 600,000 new or recurrent
strokes each year, according to statistics from the American
Heart Association. Stroke is the third leading cause of death.
It is also the main cause of long-term disability in the United
States, with 4.6 million stroke survivors alive today.
Established risk factors for stroke include standard risk
factors that lead to the development of cardiovascular disease.
Cigarette smoking elevates risk of ischemic stroke by as much
as 90%. Smoking cessation can result in a marked reduction
in stroke risk.
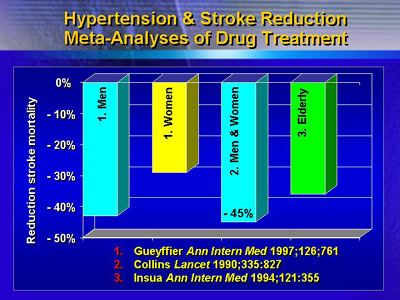
Hypertension at least doubles risk of stroke, and it is
undertreated in Western countries. 27% of Americans have hypertension.
Only 23% reach goal levels through treatment. Drug treatment
of hypertension can reduce stroke mortality by as much as
45%, regardless of other risk factors.
Diabetes increases stroke risk by 40% to 70%. Unfortunately,
several randomized studies do not show that glucose control
can reduce that risk. However, diabetics have an increased
prevalence of risk factors. In the Heart Outcomes Prevention
Evaluation (HOPE) study, diabetics who received ramipril for
blood pressure control had a 33% reduction in stroke risk.
Atrial fibrillation is an important risk factor for stroke
in the elderly. A meta-analysis suggests that warfarin reduces
risk of stroke by 61% in atrial fibrillation patients.
Total cholesterol is presumed to be a stroke risk factor.
In a meta-analysis of 18 studies and other cohorts, total
cholesterol was neither protective nor deleterious to risk
of stroke. However, this was for all types of stroke. In the
Multiple Risk Factor Intervention Trial (MRFIT), there was
an inverse association between total cholesterol and hemorrhagic
stroke. On the other hand, individuals with high total cholesterol
had the highest risk of ischemic stroke.
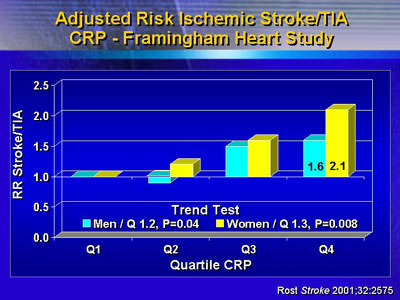
Western researchers are increasingly using subclinical disease
markers to risk-stratify patients. For example, the Framingham
Heart Study looked at the inflammatory marker C-reactive protein
(CRP) and found a dose-response relationship. Higher CRP correlated
with higher risk of stroke at follow-up. For the highest CRP
quartile, risk had approximately doubled.
There are a number of important differences in stroke epidemiology
between East and West. For example, in China, the rate of
hemorrhagic stroke is up to 30% compared with 15% in the West.
Lacunar ischemia is more prevalent in the East, while atherothrombotic
ischemia is more common in the West. Smoking is on the rise
as a risk factor in the East, while diabetes is increasing
in the West.
However, there are more similarities than differences. Stroke
shares common antecedents and are largely due to modifiable
risk factors. It is often preventable. Importantly, both West
and East underutilize risk factor modifications such as smoking
cessation that could profoundly reduce the incidence of this
disease.
|