|
There has been an overall decrease
in stroke mortality in Japan. However, Dr. Omae said that
the incidence rates of lacunar infarction and cerebral hemorrhage
are still higher than in Western countries. He also discussed
specific lifestyle and medical risk factors for cerebral infarction.
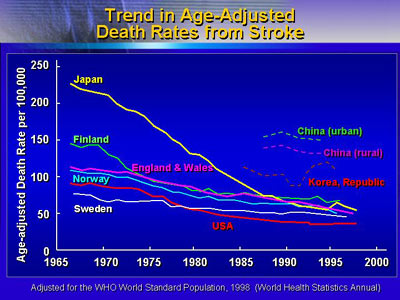
In 1965, age-adjusted stroke death rates in
Japan were more than 200 per 100,000 persons, according to
statistics from the World Health Organization. At that same
time, stroke rates were much lower in Western countries such
as Sweden and the United States.
Vital Statistics in Japan show that there
was a sharp decline in stroke mortality between 1965 and 1990
and has been leveled off thereafter. This is mainly due to
a decrease in mortality due to cerebral hemorrhage; Today,
the death rate from stroke in Japan is not particularly high
compared with those in western countries.
Several factors could be contributing to the precipitous decline
in stroke mortality in Japan. The reduction in fatal stroke
could be due to better control of hypertension or to improvement
in nutritional conditions. It could also be due to improved
care in the acute stage of stroke.
Certain stroke subtypes such as lacunar infarction
are more common in Japan than in Western countries. One large,
long-term Japanese population study provided data on incidence
of stroke by type. The study investigators reported a 45 incidence
of lacunar infarction in cases that occurred between 1961
and 1993. Another study looking at hospital admissions in
Japan between 1978 and 1991 confirmed a high incidence of
lacunar infarction. In comparison, reported lacunar infarction
rates in the United States and Switzerland have ranged from
12% to 20%.Cerebral hemorrhage rates were 20% and 22%, respectively,
in the Japanese population and hospital admission studies.
Reported rates of cerebral hemorrhage in the United States
and Switzerland are 11% to 12%.
The incidence of each stroke subtype in Japan
may be changing over time. Some data suggest an increase in
atherothrombotic infarction and cardioembolic infarction,
with a reciprocal decrease in lacunar infarction.
The Japanese population study described above
is a long-term, prospective evaluation in a rural town, Hisayama,
that is adjacent to Fukuoka. The evaluation has taken place
from 1961, when the population was approximately 6,500, to
the present (population 7,500). Researchers evaluated only
individuals at least 40 years of age in 3 separate time periods.
80% who died during the study period came to autopsy to identify
the cause of death.
Investigators noted a reduction in stroke
incidence between the earliest cohort and the second and third
cohorts. There was no change in incidence of ischemic heart
disease. Of stroke subtypes, both cerebral infarct and cerebral
hemorrhage declined in incidence from the first to second
cohort. There was no change in subarachnoid hemorrhage.
|
Change in Incidence of
Cardiovascular Disease
Hisayama 3 cohorts (aged 40 and over)
|
|
I
Cohort
(1961-69)
n=1,618 |
II
Cohort
(1974-82)
n=2,038 |
III Cohort
(1988-96)
n=2,637
|
| Stroke |
|
Infarction
Hemorrhage
Subarachnoid hemorrhage |
|
|
|
|
| Ischemic
heart disease |
| |
Myocardial infarction |
| |
Sudden death |
|
|
|
|
Incidence rate: per 1,000 year
|
(Fujishima 1999) |
| * p<0.05 vs. Cohort I |
|
|
The investigators also looked at incidence
of cerebral infarction by blood pressure group: normotensive,
borderline hypertensive, and hypertensive. Stroke incidence
increased with higher blood pressure for both men and women.
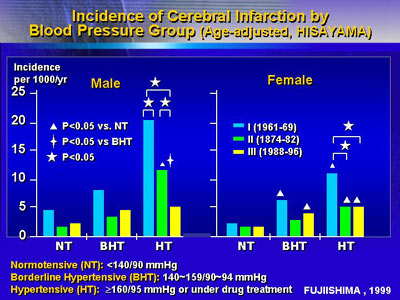
Hypertension occurred in 28% of men and 24%
of women in the first cohort. The frequency of it decreased
significantly for men in the second and third cohorts (24%
and 23% respectively) but not significantly for women (24%
and 21%).
Frequency of metabolic abnormalities increased
over time despite the decrease in stroke incidence. The rate
of obesity was relatively low in the earliest cohort, and
significantly higher in both the second and third cohorts.
Similarly, there were significant increases in hypercholesterolemia
and abnormal glucose tolerance tests over time.
The incidence of lacunar infarction varied
according to level of blood pressure. In individuals not receiving
antihypertensive drugs, there was a stepwise increase in incidence
of lacunar infarction starting at blood pressures of 140/90
mmHg and higher.
Multivariate analysis revealed that risk factors
for cerebral infarction varied by subtype. Smoking was significant
only for lacunar infarction. Only age and systolic blood pressure
were significant for atherothrombotic infarction. Findings
were fundamentally the same for men and women. Results for
men are as follows:
|
Multivariate RRs and 95% CIs of Risk Factors
for Cerebral Infarctionand its Subtypes
for Men in the Hisayama Study, 1961-93
Risk
Factor |
Cerebral
Infarction
n=144 |
Lacunar
Infarction
n=81 |
Atherothrombotic
Infarction
n=29 |
Embolic Infarction
n=31 |
| Age
|
2.2** |
2.2**
|
2.7**
|
2.2**
|
| Systolic
blood pressure |
1.2** |
1.2**
|
1.3** |
|
| Left
ventricular hypertrophy |
1.6* |
|
|
|
| ST
depression |
2.6** |
3.7** |
|
|
| Atrial
fibrillation |
3.7** |
|
|
17.8** |
| Impaired
glucose tolerance (IGT) |
1.5* |
2.0**
|
|
|
| Smoking
habits |
|
2.2
|
|
|
| All
risk factors except for age are the time-dependent
covariates. Values are RRs.
** p<0.01
* p<0.05
・Age risk for an increase of 10 years
・Systolic blood pressure risk for an increase
of 10 mmHg
(Tanizaki et al: Stroke 2000;3:2616)
|
|
The findings of the Hisayama study provide valuable insight
into the character of stroke in Japan over time. Although
much of Japanese lifestyle has become westernized, the risk
factors and the clinical profile of stroke have not been as
westernized.
|