|
Researchers now recognize that atherosclerosis
is an inflammatory disease. Dr. Libby and other investigators
have shown in animal studies that lipid lowering therapy reduces
inflammation. This may stabilize plaques and reduce the incidence
of cardiac events.
Inflammation plays a key role in the subclinical phases
of atherosclerosis. The early phases involve recruitment of
inflammatory cells. To initiate formation of an atheromatous
plaque, something must recruit mononuclear phagocytes to the
cells of the endothelial surface. Normally, mononuclear phagocytes
resist prolonged contact these cells.
Researchers now know there are a series of molecules that
allow adhesion of white blood cells to the endothelial cells.
One such molecule that has been of particular interest is
vascular cell adhesion molecule-1 (VCAM-1). Endothelial cells
do not normally express VCAM-1, but proinflammatory mediators
such as cytokines can induce production of this molecule.
Mice that have a mutation influencing VCAM-1 function have
impaired atheroma initiation, providing genetic evidence that
this molecule is indeed important for early atherogenesis.
After a white blood cell has adhered to the endothelium,
directed migration into the artery wall can occur. Chemokines,
which are chemoattractant cytokines, cause this directed migration.
One chemokine in particular is monocyte chemoattractant
protein-1 (MCP-1). It has produced great interest among researchers
because it is a potent chemoattractant for both monocytes
and lymphocytes. Endothelial and smooth muscle cells in the
area where lesions are going to form can produce this chemokine.
Dr. Libby and colleagues have shown that mice with a defect
in MCP-1 have impaired atherogenesis.
Adhesion and directed migration set the stage for development
of the atherosclerotic lesion itself. The phenotype of the
white blood cell changes from that of the usual blood monocyte
to that of a tissue macrophage. It also expresses scavenger
receptors that allow it to engulf modified lipoprotein particles.
Researchers believe macrophage colony stimulating factor
(M-CSF) is an important mediator of the inflammatory process.
Endothelial cells can produce this potent monocyte activator,
which localizes in human and experimental atheromatous plaques.
These inflammatory processes can help explain much of the
benefit of current effective therapies for atherosclerosis
such as lipid reduction with diet or statins.
Angiographically monitored statin studies show a large disparity
between the degree of improvement in lumen size and the patient's
clinical benefit. Although lipid lowering increases the lumen
only slightly, the clinical benefit is substantial. Thus,
the functional state of the plaque may be as important as
the size or degree of luminal encroachment.
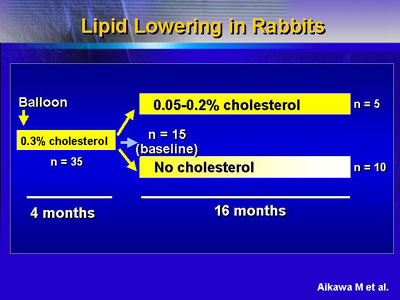
Studies of cholesterol-fed rabbits suggest a mechanism through
which lipid lowering could influence the risk that a particular
lesion may cause an acute coronary syndrome.
In one experiment, researchers created lesions in rabbits
with balloon injury and high cholesterol feeding. Some rabbits
stayed on the diet for 16 months, while others shifted to
a low cholesterol diet, allowing their hypercholesterolemia
to subside.
Baseline evaluation of the lesions revealed that smooth
muscle cells formed a fibrous cap bordering the lumen and
at the base of the plaque. In the lipid core of the lesions
were abundant macrophages. The rabbit plaques also expressed
the enzyme collagenase (MMP-1), which researchers believe
can weaken plaque and precipitate a thrombotic complication.
Returning rabbits to a normal diet seemed to have an anti-inflammatory
effect. There were many fewer macrophages. There was a decrease
in collagenase and a reciprocal increase in intimal collagen,
suggesting a more stable plaque. In addition, there was a
decrease in tissue factor, suggesting lower thrombogenicity.
Researchers have extended these studies to illustrate an
decrease in oxidative stress as cholesterol decreases. Oxidized
low-density lipoprotein cholesterol levels also decrease,
as do levels of VCAM-1, the molecule important for recruiting
monocytes. There is also a decrease in endothelial nitric
oxide synthase, the enzyme that makes nitric oxide.
Now, preliminary observations suggest dietary cholesterol
lowering in this animal model yields fewer microvessels in
the plaque. This subject will require more study. However,
evidence to date strongly suggests that inflammation is an
integral part of the atherogenic process and that lipid lowering
is an anti-inflammatory therapy.
|