|
Dr. Rabinovitch described the contribution
of her laboratory to the body of research on the role of elastase
inhibition in vascular disease. Studies of animal models suggest
that elastase inhibitors can prevent or even reverse vascular
disease resulting from inflammation.
The research program of Dr. Rabinovitch and colleagues focuses
on the pivotal role of an elastin degrading enzyme (which
they call an endogenous vascular elastase) in the pathobiology
of vascular disease.
Release of this enzyme has multiple effects. The breakdown
products of elastin, elastin peptides, elicit the accumulation
of inflammatory cells. These cells then penetrate the vessel
lumen, releasing their own elastases and matrix metalloproteinases.
This results in amplification of the proteolytic response.
Growth factors normally stored in an inactive form are also
released as part of this chain of events.
Inhibiting the activity of endogenous vascular elastase may
prevent the events of vascular injury. This research group
initially used elastase inhibitors to treat experimental rodent
models of pulmonary hypertension.
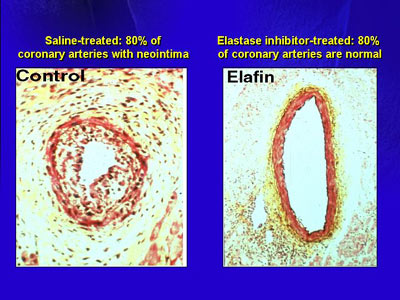
The investigators first explored the hypothesis that a very
aggressive form of coronary artery disease that occurs after
heart transplant may be susceptible to treatment with elastase
inhibitors. In a rabbit heart transplant model, they found
extensive neointimal lesions that partially or almost completely
occluded the vessel lumen. In contrast, in animals treated
with elafin, a naturally occurring human elastase inhibitor,
80% of arteries maintained a pristine form.
After demonstrating this, the researchers studied elafin
in settings where inflammation can contribute to vascular
disease. In rabbits, they interposed the jugular vein in the
carotid arterial position and infused that vein with a recombinant
form of the elastase inhibitor elafin delivered by gene therapy.
In this model, they assessed inflammation at 48 hours. They
easily detected an inflammatory response in a control arm,
while very few inflammatory cells were evident in the veins
of the animals they treated with gene therapy.
When they assessed intimal thickening, it was appreciable
in veins perfused with saline as a control. In contrast, there
was a marked reduction in intimal thickening in vein grafts
treated with elafin gene therapy (up to 50% in some cases).
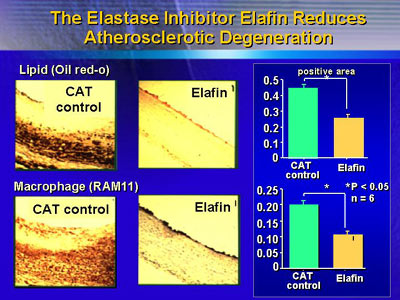
The neointima in the vessels treated with elafin might also
resist atherosclerotic degeneration, investigators reasoned.
Toward this end, they gave animals a high cholesterol diet
for 3 months after elafin gene therapy and interposition of
vein grafts. In control vessels, they found dense accumulation
of lipid, while vessels from the gene therapy arm had only
about 50% as much accumulation.
Further research in mice suggested that propensity to develop
vascular disease is partially dependent on an individual's
ability to mount an anti-elastase response, perhaps by generating
elastase inhibitors such as elafin endogenously.
In an experimental model of pulmonary hypertension, the investigators
demonstrated that elastase inhibitor therapy, using 2 oral
products developed by a pharmaceutical company, provided a
survival advantage at 1 and 2 weeks in mice that they treated.
Then they measured levels of pulmonary artery pressure and
found regression of pulmonary hypertension in comparison with
controls.
Because this model suggested that elastase inhibitors could
prevent or even reverse vascular disease resulting from inflammation,
they evaluated the effect of these agents in the inflammatory
process in myocardium. In a mouse model of myocarditis, untreated
animals had extensive inflammatory cell infiltration, and
even calcification. Mice who received continuous elastase
inhibitor therapy showed little evidence of inflammation.
In further observations, they found that treatment of a myocardial
infarct model suggested improved healing of heart tissue.
More recently, investigators found that elastase inhibitors
improve structural and functional healing following myocardial
infarction, probably by repressing inflammation and fibrosis.
These study results represent the findings of only one research
group. It is the contributions of other research groups, along
with this one, that will create a more complete picture of
the potential role of elastase inhibitors in vascular disease,
Dr. Rabinovitch said.
|