|
Pharmacologic therapy is often ineffective
against atrial fibrillation and can lead to side effects, recurrent
cardioversions, and hospitalizations. For those reasons, development
of non-pharmacologic approaches has been an important research
area. Two of the most important are defibrillation and ablation.
Early approaches to non-pharmacologic therapy for atrial
fibrillation mainly addressed rate control. These approaches
include modification of the atrioventricular node, or more
commonly, atrioventricular node ablation with implantation
of a permanent pacemaker.
Newer approaches have attempted to increase the probability
of maintaining sinus rhythm. These include adjunctive pacing,
the use of implantable defibrillators, surgical procedures,
and catheter ablation.
Traditional atrial overdrive pacing may decrease the likelihood
of atrial fibrillation, but results of studies have been mixed.
Although some studies suggest a reduction of up to 60%, others
show no effect.
|
Effect of Atrial Overdrive Pacing on AF Prevention
| Study |
Patients
(n) |
Results |
| Lam,
2000 |
15 |
No
effect |
| PROVE,
2000 |
78 |
34%
decrease |
| Ricci,
2001 |
61 |
No
effect overall;Decrease if DDDR % pacing is decreased |
| Israel, 2001 |
325 |
No
effect |
| Gold, 2001 |
75 |
No
effect |
| ADOPT-A, 2001 |
399 |
60%
vs 45% reduction |
|
Implantable combined atrial/ventricular defibrillators allow
for dual-chamber pacing. They provide therapy for both ventricular
and atrial tachyarrhythmia through anti-tachycardia pacing
and both low- and high-energy shocks.
In most cases, atrial fibrillation thresholds are reasonable
with the lead configurations in standard implantable atrial
defibrillators. The energy required to terminate defibrillation
is in the range of 4 to 7 joules. However, this amount of
energy can still cause a considerable amount of pain. For
this reason, researchers hoped novel pacing therapies could
further decrease episodes of atrial fibrillation.
To test this, investigators studied the effects of a Jewel
AF implantable defibrillator in 537 patients with ventricular
arrhythmia and documented history of atrial tachyarrhythmias
in most cases. This device uses 3 different overdrive atrial
pacing methods and discriminates between atrial tachycardia
and atrial fibrillation based on length and regularity of
cycle. Investigators found that atrial pacing terminated almost
half (48%) of all episodes of atrial tachycardia and atrial
fibrillation. Unfortunately, many patients continued to require
shocks.
Another recent trial of the Jewel AF device showed a decrease
in atrial fibrillation burden from 53 hours per month (pacing
therapies off) to 6.2 hours per month (pacing therapies on).
However, the benefit accrued to just about 25% of patients,
with most of the rest showing relatively little change. The
median change was less than 1 hour per month.
These trials show that the application of pacing algorithms
work to a modest degree, but that many patients continue to
have episodes.
Curing atrial fibrillation would be preferable to treatment
that simply manages symptoms. For that reason, there have
been many studies evaluating ablation strategies, mostly occurring
in the pulmonary veins.
The results of ablation procedures are quite successful,
both for improving clinical outcomes and quality of life.
For isolation procedures, the cure rate is about 70% to 80%
in some series. Variables such as age, gender, left ventricular
ejection fraction, or duration of atrial fibrillation do not
appear to have an effect on the success of the procedure.
|
Pulmonary Vein Isolation of
Paroxysmal Atrial Fibrillation
| Study |
Patients
(n) |
Procedure |
Cured |
| Marrouche, 2002 |
111 |
Isolation
|
88% |
| Oral, 2002 |
58 |
Isolation |
70% |
| Pappone, 2001 |
179 |
Isolation |
85% |
| Wharton, 2000 |
113/67 |
Focal/Isolation
|
72%/75% |
| Haissaguerre, 2000 |
225 |
Focal/Isolation
|
70% |
| Chen, 1999 |
79 |
Focal |
86% |
| Gerstenfeld,
2001 |
71 |
Focal |
33% |
|
Downsides of ablation procedures include cardiac perforation,
pulmonary vein dissection, vascular damage and stroke, among
others. The most worrisome complication is pulmonary vein
stenosis. Severe stenosis occurs in far less than 5% of cases,
but up to 25% of patients have it to some degree. Symptoms
can include severe dyspnea and coughing up blood from the
respiratory tract.
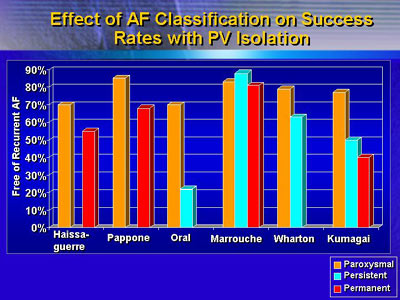
Furthermore, this therapy appears to be somewhat more effective
in patients with paroxysmal episodes of atrial fibrillation
as opposed to persistent or chronic atrial fibrillation. It
would be desirable to have ablation procedures also applicable
to persistent and chronic atrial fibrillation.
In the future, it is likely that both surgical and catheter
ablation approaches will develop not just for treatment of
paroxysmal cases, but also for persistent and even chronic
atrial fibrillation. For now, the front line treatment for
all patients is still pharmacologic therapy.
|