|
Moving beyond empiricism in the treatment
of atrial fibrillation requires a synthesis of data from animal
models, observational human data, and from prospective, clinical
trials, Dr. Falk said in a plenary session presentation. He
presented an argument for separating atrial fibrillation from
atrial flutter as arrhythmia under study and for developing
prospective clinical trials on the possible role of adjunctive
therapies.
International consensus guidelines from 2001 recommend giving
specific antiarrhythmic drugs according to the patient's underlying
pathology. Patients with no clinical heart disease have a
wide variety of options. On the other hand, patients with
hypertension, heart failure, or coronary disease have a much
smaller choice of drugs.
These recommendations are an important step away from empirical
treatment. However, this is not a move toward effective drugs
for specific conditions. Rather, this is an attempt to avoid
known side effects.
One safety concern is the incidence of torsades de pointes.
Physicians in the United States and elsewhere no longer favor
quinidine because of the potential for increased mortality.
Researchers presume the underlying mechanism is torsades de
pointes. Sotalol also causes torsades de pointes, but it may
be a safer drug because its effect appears to be dose related
whereas the adverse effect may not be dose related for quinidine.
Recent data suggest that clinicians could use adjunctive
therapies to block the adverse effect of these two drugs.
In a rabbit model, use of verapamil almost completely eliminated
the risk of erythromycin-induced torsades de pointes.
In an unpublished European clinical trial, researchers tried
use of verapamil in conjunction with quinidine. There were
no cases of documented torsades de pointes in 88 placebo-treated
patients compared with a 2.3% incidence in 380 patients who
received sotalol. Interestingly, there were no cases of torsades
de pointes in 377 patients on quinidine and verapamil.
| Incidence
of Torsades de Pointes:
Quinidine + Verapamil vs. Sotalol
| - |
Placebo |
Quinidine+
Verapamil |
Sotalol |
| Patients
(n) |
88 |
377 |
383 |
| Torsades
cases |
0 |
0
|
9 |
| Percent |
0 |
0 |
2.3 |
Vester
et al., Eur Heart J. Abstr. Suppl. 2002; 4: 486.
|
One obstacle in moving away from empiricism is that many
trials have lumped together patients with atrial fibrillation
and those with atrial flutter. This is probably not appropriate
for analysis, particularly with the newer antiarrhythmic drugs,
Dr. Falk said.
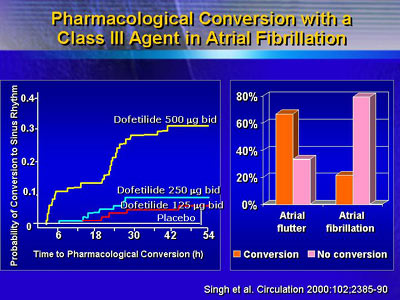
One example comes from a study of dofetilide for the conversion
and maintenance of sinus rhythm. The most effective dose had
a 30% chance of converting arrhythmia into sinus rhythm. However,
when the data are broken down by specific arrhythmia, the
conversion rate for atrial flutter was 60% in contrast to
just over 20% for atrial fibrillation.
In the dofetilide study, probability of patients remaining
in sinus rhythm dropped rapidly in the first few weeks. After
that, the loss of sinus rhythm was much slower. Atrial remodeling
due to atrial fibrillation may be responsible for the early
and rapid decline.
Verapamil appears to maintain sinus rhythm after cardioversion.
In one study, patients received either propafenone alone or
with verapamil. Patients who received propafenone alone had
a much greater rate for loss of sinus rhythm than those treated
with propafenone and verapamil.
Another study compared the maintenance of sinus rhythm in
patients receiving amiodarone, propafenone, or sotalol. The
propafenone and sotalol groups had a similar rapid loss of
sinus rhythm early in the study, whereas amiodarone treatment
seemed to mimic the effect researchers showed in the study
with verapamil plus propafenone.
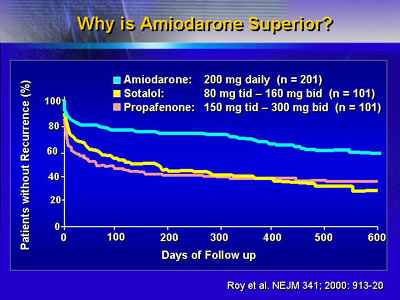
It is not clear why amiodarone would be superior to other
antiarrhythmic agents. However, one researcher presented an
abstract at AHA 2002 suggesting that amiodarone may be effective
in preventing remodeling, and hence early loss of sinus rhythm
in converted patients.
A more recent approach is to examine the effect of amiodarone
plus irbesartan on maintenance of sinus rhythm. A small, unblinded
study showed that patients who received amiodarone had a significantly
higher recurrence rate than the patients who received amiodarone
plus irbesartan. Dr. Falk said it is not clear yet whether
the combination does indeed work better than amiodarone alone.
For the future, researchers will have to rethink the role
of antiarrhythmic therapy for atrial fibrillation. One important
goal is to conduct large, prospective, randomized studies
of adjunctive therapies.
|