Researchers
demonstrated a strong association between circulating levels
of matrix metalloproteinases (MMP) and Tumor Necrosis Factor-Alpha
(TNF-α) in patients with idiopathic dilated cardiomyopathy.
Carvedilol, the nonselective beta-blocker, reduced circulating
levels of both MMPs and TNF-α. This reduction in both circulating
MMPs and TNF-α levels may be beneficial effects of carvedilol
in this condition.
Research has shown that increased matrix metalloproteinases
(MMP) activity occurs in idiopathic dilated cardiomyopathy.
In addition, experimental studies show that the proinflammatory
cytokine Tumor Necrosis Factor-Alpha (TNF-α) stimulates myocardial
MMP activity, leading to degradation of the extracellular
matrix in the myocardium. However, there have been few clinical
studies of the relationship between circulating MMP and TNF-α
levels in idiopathic dilated cardiomyopathy.
Previously, Dr. Ohtsuka and colleagues reported an increase
in circulating TNF-α in patients with idiopathic dilated cardiomyopathy.
They showed that beta-blockers could attenuate this increase.
Here at ACC, the researchers further clarified the relationship
between circulating MMPs and TNF-α.
The researchers studied 34 patients (6 women and 28 men,
mean age 52 years) with a diagnosis of idiopathic dilated
cardiomyopathy. 19 patients were in New York Heart Association
functional class II, 12 patients in class III, and 3 patients
in class IV. Researchers also established a control group
of 10 age matched subjects who had no evidence of organic
cardiac disease or cardiac dysfunction.
Twenty of the 34 patients were poor responders to treatment
with angiotensin II type 1 receptor blockers for at least
6 months. These 20 patients received the oral nonselective
beta-blocker carvedilol in addition to other combination therapy.
Carvedilol treatment started at 2.5 mg twice daily, with increasing
doses at weekly intervals for 8 weeks. The mean final dose
of carvedilol was 19.2 mg.
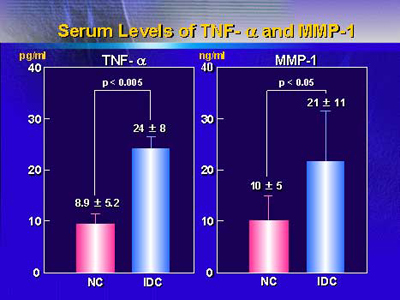
As shown in the following figure, patients with idiopathic
dilated cardiomyopathy had significantly higher serum TNF-α
and MMP-1 levels versus control subjects. Serum levels of
MMP-3 and MMP-9 were also significantly higher versus controls.
In patients with idiopathic dilated cardiomyopathy, there
was a significant correlation between serum levels of MMP-9
and TNF-α (r=0.764, p=0.01). This is the first clinical observation
of the relation between circulating levels of MMPs and TNF-α
in patients with this condition.
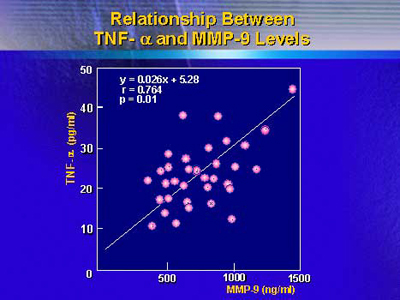
Levels of MMP-1 and MMP-3 did not correlate significantly
with TNF-α levels in patients with idiopathic dilated cardiomyopathy.
However, there was a significant correlation between MMP-1
and BNP levels (r=0.647, p=0.022). In addition, serum MMP-9
levels correlated positively with plasma norepinephrine levels.
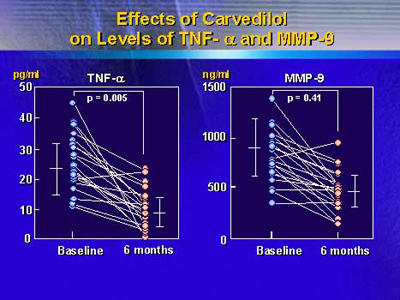
Notably, the illustration below shows that carvedilol modulated
the increase in TNF-α and MMP levels in patients with idiopathic
dilated cardiomyopathy after 6 months of treatment. High levels
of MMP-1 and MMP-9 decreased significantly, though MMP-3 levels
did not change.
Dr. Ohtsuka and colleagues said the most important finding
was the close relationship between increased circulating MMP-9
levels and increased TNF-α levels in patients with idiopathic
dilated cardiomyopathy. The researchers believe that in patients
with this condition, increased TNF-α could be one molecular
trigger for induction of circulating MMPs, especially MMP-9.
Therefore, they suggest that in patients with idiopathic dilated
cardiomyopathy, carvedilol may downregulation TNF-α, thereby
reducing the amount of circulating MMPs.
|