This
large clinical trial looked at coronary event risk in hypertensive
patients with normal or mildly elevated cholesterol. Study subjects
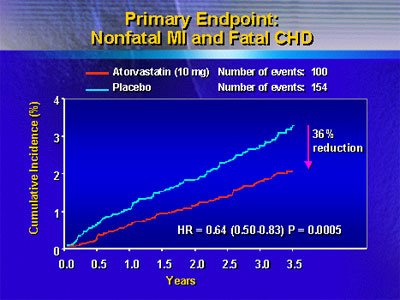
had 36% fewer nonfatal myocardial infarctions or fatal coronary
events when they took atorvastatin in addition to antihypertensive
therapy. The finding suggests that adding a statin to a regimen
for lowering blood pressure could prevent a significant number
of coronary events.
One important unresolved problem in the management of blood
pressure is elevated risk of coronary heart disease (CHD).
Dyslipidemia is highly prevalent in hypertensive patients.
However, there are a number of patients not deemed dyslipidemic.
To date, there have been no major trials addressing the potential
impact of lipid lowering on CHD incidence in hypertensives
without dyslipidemia.
Anglo-Scandinavian Cardiac Outcomes Trial (ASCOT) is a randomized,
controlled trial that sought to evaluate the role of cholesterol
lowering in hypertensive patients who have normal or mildly
elevated cholesterol levels. Recruiting centers included almost
700 general practices in Scandinavian countries and 32 regional
centers in the United Kingdom.
The study included almost 20,000 patients with high blood
pressure. Investigators randomized the patients to receive
1 of 2 blood pressure lowering regimens: a beta blocker plus
a diuretic, or a calcium channel blocker plus an ACE inhibitor.
In addition, 10,305 patients participated in a second part
of the study. These patients all had total cholesterol levels
less than 250 mg/dL. Current treatment guidelines in the United
States and Europe consider 250 mg/dL to be normal or slightly
elevated. Investigators randomized these patients to receive
atorvastatin 10 mg or placebo. Investigators refer to this
second part as the lipid lowering arm of the trial.
The primary endpoint of the lipid lowering arm was non-fatal
myocardial infarction or fatal CHD. Investigators expected
a 30% relative effect on this endpoint versus placebo.
Of the study participants in the lipid lowering arm, 81%
were men, and the mean age was 63 years. All had hypertension
and at least three other risk factors for CHD. The Data Safety
Monitoring Board stopped the trial early because of a significant
reduction in the primary endpoint. At the point of closure,
there was a median follow-up of 3.3 years.
Analysis revealed that the patients achieved very good blood
pressure control in both the atorvastatin and placebo control
group. Blood pressure at follow-up was 138/80 mmHg, down from
164/95 mmHg at baseline. Total cholesterol, similar in the
atorvastatin and placebo group at baseline; at 3.3 years,
there was a 1.1 mmol/L difference favoring atorvastatin.
Primary endpoint analysis showed a 36% reduction in non-fatal
myocardial infarction and fatal CHD at 3.3 years in the atorvastatin
arm. Investigators noted that the difference between atorvastatin
and placebo emerged earlier than in other major statin trials.
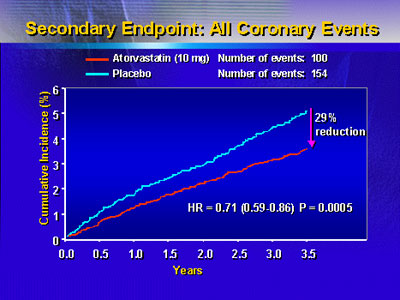
In addition, investigators reported significant reductions
in fatal or non-fatal stroke (27%, p=0.0236), all cardiovascular
events and procedures (21%, p=0.0005) and all coronary events
(29%, p=0.005). There was a trend toward reduction in total
mortality favoring atorvastatin, but this did not reach statistical
significance.
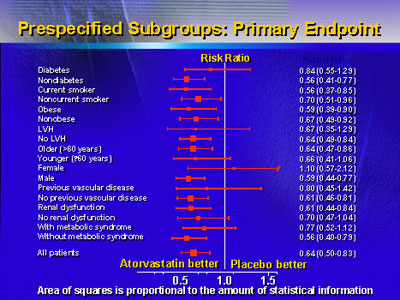
Investigators performed a number of prespecified subgroup
analyses. They found no difference in outcomes. This suggests
the benefit of atorvastatin in treated hypertensives applies
to a variety of subgroups, including patients with diabetes,
smokers, obese individuals, and patients with renal dysfunction.
Safety evaluations showed no significant difference in the
number of fatal cancers, serious adverse events or liver enzyme
abnormalities between atorvastatin and placebo. There was
one case of rhabdomyalysis in the atorvastatin group. However,
this occurred in a severely alcoholic patient who had a recent
febrile illness.
Investigators said the reductions in major adverse cardiac
events they observed are large and notable because they occurred
within a relatively short follow-up period. Had follow-up
continued to a median of 5 years, investigators expect they
would have observed a 50% reduction in CHD events.
Furthermore, the benefit of the statin occurred much earlier
than in many other statin trials. It is not clear whether
the early benefit occurred because of the lipid lowering effect
of the statin or some Investigators believe the bulk of evidence
so far suggests early reduction in LDL cholesterol is a very
important contributor to this effect.
The challenge for cardiologists is to incorporate a new
therapy into the antihypertensive armamentarium. Already,
many patients could have better blood poorly controlled blood
pressure. This is partly because they do not adhere to potentially
effective treatment regimens, and partly because physicians
are not treating hypertension aggressively. However, investigators
believe doctors should not exclude statins as a potentially
effective treatment for primary prevention of CHD in hypertensive
patients.
|