| The
AFFIRM trial compares mortality risk among approximately 4,000 atrial
fibrillation patients randomized to the popular rhythm control approach
or to rate control. Primary results of this large trial show fewer
deaths in the rate control arm. This result did not quite achieve
statistical significance. However, the results suggest rate control
is at least as beneficial as rhythm control in these patients. In
addition, the rate control approach may be more cost-effective and
may provide better quality of life.
The 2 treatment strategies for patients with recurrent atrial fibrillation
that has not yet become permanent are sinus rhythm control or ventricular
rate control.
Most North American physicians prefer to start with rhythm control.
Presumed benefits include lower risk of stoke, improved survival,
and fewer patient symptoms. Also, some physicians feel they can
discontinue anticoagulation if treatment results in maintenance
of sinus rhythm. These presumed benefits remain largely unproven.
Atrial Fibrillation Follow-Up Investigation of Rhythm Management
(AFFIRM) is the largest investigation to date of rate versus rhythm
control in atrial fibrillation. It is also among the first using
mortality as a primary endpoint.
Patients in the AFFIRM trial had ECG documented atrial fibrillation.
They had to have at least 1 risk factor for stroke or death, such
as advanced age, hypertension or diabetes. At ACC, investigators
presented follow up available for 98% of the 4,060 patients they
enrolled. The mean follow up was 3.5 years. There were no differences
in patient characteristics between the rate and rhythm control arms.
After randomization to rate or rhythm control, investigators chose
the therapy they felt was appropriate. They used non-pharmacologic
therapies if pharmacologic therapies were unsuccessful. Patients
could cross over from rate control to rhythm control, and vice versa.
Initial therapy in the rate arm included digoxin, beta-blockers
and calcium channel blockers. The most common initial therapy in
the rhythm control arm was amiodarone or sotalol. During the study,
there were frequent changes in therapy.
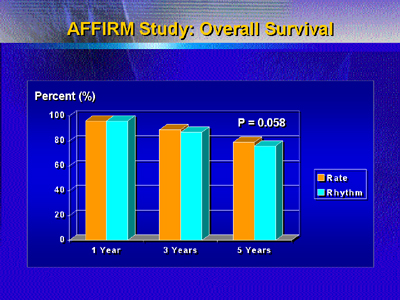
Primary results of AFFIRM showed a late trend toward increased
all cause mortality in the rhythm control arm. Beginning at 18 to
24 months, mortality curves began to separate in favor of the rate
control arm. At the end of follow-up, there were 306 deaths in the
rate control arm and 356 deaths in the rhythm control arm (P = 0.058).
Adverse Events
|
-
|
Rate Control
|
Rhythm Control
|
P-Value
|
|
Death
|
306 (26%)
|
356 (27%)
|
0.058
|
|
Torsades de pointes VT
|
2 (0.2%)
|
13 (0.8%)
|
0.004
|
|
Sustained VT/VF cardiac arrest
|
24 (1.7%)
|
18 (1.2%)
|
0.355
|
|
Bradycardia cardiac arrest
|
2 (0.1%)
|
13 (0.8%)
|
0.004
|
|
Intracranial bleed
|
31 (2.0%)
|
29 (2.1%)
|
0.799
|
|
Major hemorrhage
|
106 (7.6%)
|
96 (6.9%)
|
0.473
|
|
Patients hospitalized after baseline
|
1,218 (70%)
|
1,375 (78%)
|
<0.001
|
|
Ischemic stroke
INR ≧ 2.0
INR < 2.0
Not taking warfarin
AF at time of event
|
79 (5.7%)
24 (30%)
28 (35%)
26 (33%)
45 (69%)
|
84 (7.3%)
18 (22%)
17 (20%)
48 (58%)
25 (36%)
|
0.680
|
Event rates derived from Kaplan-Meier analysis
Interestingly, strokes were most common in patients who stopped
anticoagulation or received a sub-therapeutic dose. This suggests
it may be important to maintain anticoagulation therapy in patients
with atrial fibrillation and stroke risk factors.
Hospitalizations after baseline were significantly less frequent
in the rate control arm. Because hospitalization can be a surrogate
for cost, rate control may be more cost effective than rhythm control.
There were significantly fewer cases of bradycardia cardiac arrest
and torsades de pointes in the rate control arm. There were no significant
differences in intracranial bleeding, major hemorrhage, or sustained
ventricular tachycardia/ventricular fibrillation cardiac arrest.
The AFFIRM study demonstrates that rate control is an effective
primary therapy. The results did not support any of the presumed
benefits of maintaining sinus rhythm. The trends in mortality and
hospitalization may actually be benefits of the rate control approach.
|