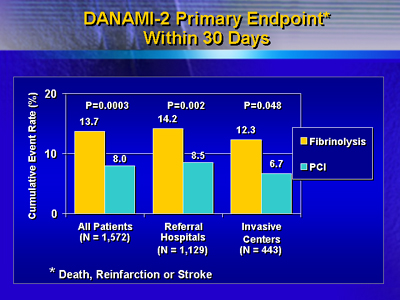
| In
this study, investigators treated ST elevation myocardial patients
with front loaded tPA, or had them transported to an invasive center
for angioplasty. Results show a relative risk reduction of more than
40% at 30 days for patients who received the interventional procedure.
The results suggest delayed percutaneous coronary intervention is
preferable to immediate thrombolysis, even if patients must be transported
a long distance for the procedure.
The Danish Multicenter Randomized Trial on Thrombolytic Therapy
versus Acute Coronary Angioplasty in Acute Myocardial Infarction
(DANAMI) study included 1,572 patients enrolled at 5 invasive centers
and 24 referral hospitals in Denmark. The service areas of the 29
hospitals cover 62% of Denmark's 5.4 million inhabitants.
Investigators in DANAMI randomized ST elevation myocardial infarction
(MI) patients to either fibrinolysis or percutaneous coronary intervention
(PCI) with stenting. The fibrinolysis regimen was 100 mg front-loaded
tPA.
Patients enrolled directly in the invasive centers received fibrinolysis
or the interventional procedure. Patients enrolled at referral hospitals
received fibrinolysis, or else ambulance transfer to an invasive
center for a procedure. The maximum transport distance possible
was about 95 miles. Transfer time could not exceed 3 hours.
The primary endpoint was the composite of death, reinfarction or
disabling stroke at 30 days. For all 1,572 patients, incidence was
8% in the PCI arm, and 13.7% in the thrombolysis arm (P = 0.0003).
The number needed to treat to avoid one event was 18. Further analysis
revealed a significant reduction in reinfarction (1.6% for intervention
vs. 6.3% for fibrinolysis, P < 0.0001).
DANAMI-2: Primary Endpoints within 30 Days (n = 1,572)
| |
Fibrinolysis
|
PCI
|
P value
|
| Death |
7.6 %
|
6.6 %
|
0.35
|
| Reinfarction |
6.3 %
|
1.6 %
|
< 0.0001
|
| Disabling
Stroke |
2.0 %
|
1.1 %
|
0.15
|
| Combined |
13.7 %
|
8.0 %
|
0.0003
|
For patients enrolled at the referral hospitals only, results also
favored transport to intervention over immediate thrombolysis. The
cumulate event rate at 30 days was 8.5% for intervention and 14.2%
for thrombolysis (P = 0.002).
The finding was the same for the 443 patients enrolled directly
at the invasive centers, albeit not as significant, probably due
to the low number of patients in this arm. Investigators stopped
the DANAMI study before completing planned enrollment at the invasive
centers. They stopped the study because they enrolled enough patients
in the referral hospitals to determine whether transport for intervention
was preferable to thrombolysis.
Transport appears safe. There were no deaths or intubations during
transport. Incidence of atrial fibrillation, ventricular tachycardia
and ventricular fibrillation were 2.5%, 0.2% and 1.4%, respectively.
Mean transport distance was 35 miles.
These new findings confirm previous trial results suggesting primary
PCI, in an invasive center, is superior to thrombolysis. The DANAMI
study adds more to the discussion. It shows that transporting patients
from a referral hospital to an invasive center does not obviate
the benefit of the intervention vs. thrombolysis.
|