| The
issue of complete or partial revascularization following initial therapy
for acute coronary syndromes was discussed. Evidence indicates ejection
fraction (less than 40%) is a more important determinant of survival
than complete or incomplete revascularization. Patients with poor
ventricular function should be completely revascularized.
Dr. O'Neill discussed whether patients with acute coronary syndromes
should be partially or completely revascularized following initial
therapy. Patients with acute coronary syndromes, such as myocardial
infarction, present with one or more vessels occluded.
Patients who presented with single lesions were usually treated
with angioplasty. 40% of patients with complex lesions were treated
with cardiac bypass surgery. Patients with multiple lesions had
a significantly higher recurrent event rate. This was seen as a
larger number of repeat angioplasties, recurrent ischemia and cardiac
bypass surgeries.
Stent PAMI* Experience: Predictors of Mortality in Multiple Lesion
Patients
| Death 1 year |
P value
|
Odds ratio
|
95% CI
|
| 2nd lesion diagnosed |
0.0096
|
2.83
|
1.29-6.23
|
| Female |
0.0015
|
3.05
|
1.53-6.05
|
| Final TIMI ≦3 |
0.0075
|
3.17
|
1.36-7.38
|
| Ejection fraction <40% |
0.0019
|
3.00
|
1.50-5.99
|
* PAMI=Primary Angioplasty in Myocardial Infarction
Ejection fraction is a more important determinant of mortality
than complete or incomplete revascularization. Patients with preserved
ventricular function do well long-term whether they are completely
or incompletely revascularized. Patients with ejection fractions
less than 40% who are completely revascularized have less mortality
2 years after treatment. Dr. O'Neill concluded patients with poor
ventricular function should be completely revascularized. Complete
revascularization also results in a lower recurrence of angina.
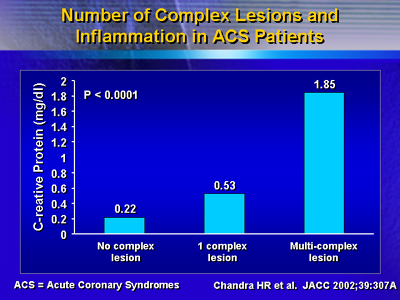
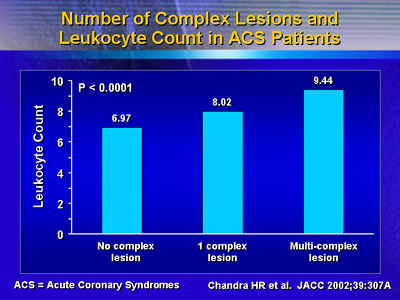
Dr. O'Neill hypothesized that coronary lesions are part of a systemic
process. To demonstrate a systemic response, Dr. O'Neill's laboratory
measured serum levels of C-reactive protein and leukocytes in patients
with single and multiple complex lesions. C-reactive protein indicates
the occurrence of a systemic inflammatory process that is not limited
to the coronary artery. The results indicate patients with multiple
lesions had higher levels of C-reactive protein and leukocytes.
Patients with multiple lesions often presented with stenosis in
other vessels. Many of these patients received multiple stents in
the same vessel. Patients receiving multiple interventions had a
lower survival rate one year later. Survival rate was affected by
a reduced ejection fraction (less than 40%) and being female. Dr.
O'Neill recommended referring these patients for cardiac bypass
surgery followed by complete revascularization.
Patients with cardiogenic shock who are treated with angioplasty
should be completely revascularized. These patients can be difficult
to manage. Intervention with multiple vessel disease and cardiogenic
shock results in 67% mortality.
When multiple vessel disease is present, an acute diffuse, systemic
inflammatory process is present. Dr. O'Neill notes the need for
systemic treatment in addition to the mechanical treatment provided
by angioplasty, stents or cardiac bypass surgery. Dr. O'Neill suggests
this combined approach may lead to increased survival.
|