| The
presence of inflammation in atherosclerotic plaques is well known.
However, contrary to popular opinion, inflammation in the coronary
vasculature correlates only with unstable angina or acute coronary
syndromes, but not with atherosclerosis itself or with ischemia or
myocardial necrosis. Many possible infectious and non-infectious causes
of vascular inflammation are being investigated.
We have known about the presence of inflammation in atheromas,
or atherosclerotic plaques, for many years. The triggers of plaque
instability may include mechanical rupture of vulnerable plaques
or inflammatory activity of the vascular wall. The effects of inflammation
in the vascular wall include prothrombotic and vasoconstrictive
effects, expression of adhesion molecules for binding of platelets
and inflammatory leukocytes, and activation of metalloproteinases,
which contribute to endothelial cell detachment, matrix degradation,
and plaque disruption. Systemic inflammatory markers in patients
with unstable angina include activated lymphocytes, monocytes, and
neutrophils, and soluble markers such as C-reactive protein, interleukin-1,
and interleukin-6.
However, contrary to the beliefs of many physicians, we have found
that the presence of active inflammation appears to be correlated
only with unstable angina or acute coronary syndromes, but not with
atherosclerosis itself or with myocardial ischemia or necrosis.
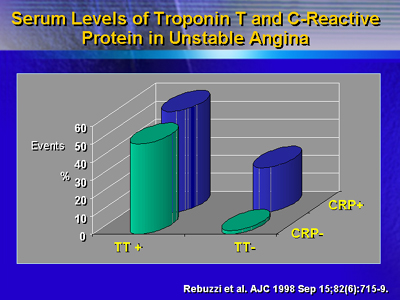
One of the best markers of inflammation is C-reactive protein,
because of its long half-life. Nevertheless, while levels of C-reactive
protein do not correlate with atherosclerosis and ischemia, they
do provide an independent prognostic indicator of infarction, even
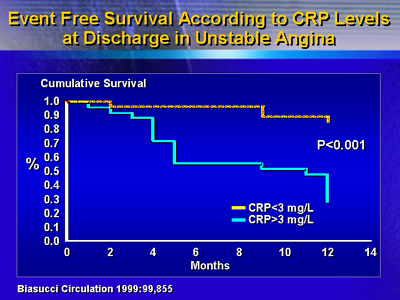
in patients who are troponin-negative. In addition, elevated C-reactive
protein levels at the time of discharge from the hospital for unstable
angina correlate strongly with lower event free survival at 1 year
post-discharge.
The causes of vascular inflammation in these patients is not clear,
and there are many possible causes being investigated. These include
infectious and non-infectious agents including bacteria, viruses,
oxidants, and toxins. There may also be an enhanced inflammatory
response to vascular trauma and myocardial necrosis, as well as
immunologic stimuli involving modified T lymphocytes. With continuing
research, the understanding of the causes of inflammation and its
coronary localization may open the way to novel therapeutic strategies.
|