| A
systematic approach for the selection of optimal medical therapy for
systolic heart failure is presented. This approach relieves volume
overload and congestive symptoms with diuretics. Once the symptoms
of congestion are relieved, digitalis therapy is started. Once stable,
the therapy of choice is angiotensin converting enzyme (ACE) inhibitors.
The addition of beta-blockers are discussed. The use of aldosterone
antagonists, amiodarone and other therapies are included.
Clinical presentation of systolic heart failure is often volume
overload and congestive symptoms. These symptoms are relieved with
diuretics. Diuretics are not recommended for long-term treatment.
Dr. Chatterjee detailed a systematic approach for the selection
of optimal medical therapy for systolic heart failure.
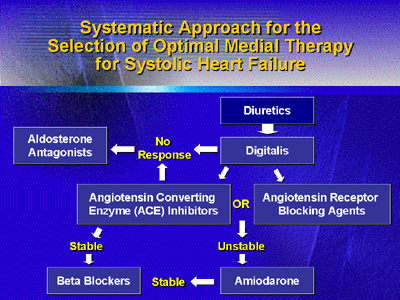
Dr. Chatterjee recommended using diuretics to relieve volume overload
and congestive symptoms. Diuretics are not recommended long-term
because they produce adverse effects such as increased levels of
norepinephrine, angiotensin and vasopressin; increased renal dysfunction;
electrolyte abnormalities and promote ventricular remodeling.
Once the symptoms of congestion are relieved, digitalis therapy
is started. Once stable, the therapy of choice is ACE inhibitors.
ACE inhibitors prevent ventricular remodeling, improve left and
right ventricular function, symptoms, quality of life and decrease
the risk of mortality. Dr. Chatterjee recommends starting ACE inhibitors
at a low dose, and measuring serum sodium. Patients with low sodium
levels can become hypotensive with this drug. If ACE inhibitors
are not tolerated, angiotensin receptor blocking agents are used.
After stabilizing a patient on triple therapy (diuretics, digitalis,
ACE inhibitors), beta-blockers are added. Beta-blockers improve
hemodynamics, left and right ventricular function, quality of life,
survival, decrease the progression of heart failure and attenuate
ventricular remodeling.
If a patient is volume overloaded and does not respond to digitalis
or ACE inhibitors, aldosterone antagonists are used. Aldosterone
inhibitors improve hemodynamics by decreasing end diastolic volume,
end systolic volume, and attenuating ventricular remodeling. Serum
sodium and potassium are monitored when aldosterone inhibitors are
used.
Patients who do not tolerate beta-blockers are started on amiodarone.
When patients are stabilized on amiodarone, they may be switched
to beta-blocker therapy. Patients with severe heart failure who
are in cardiogenic shock and present with hypotension, tachycardia
and low cardiac output, may benefit from a ventricular assist device.
Other therapies discussed by Dr. Chatterjee are the use of combined
non-glycosidic ionotropic and beta-blocker therapy. Dr. Chatterjee
suggests using these drugs separately. Dr. Chatterjee does not recommend
combining ionotropic agents and direct acting vasodilators. Other
treatments to consider are immunomodulators, immunoglobulin therapy;
and B-type natriuretic factor; their role in heart failure is unclear.
|