| A
systematic approach for the diagnosis of heart failure was presented.
This approach includes clinical history, physical exam and laboratory
tests. A complete clinical history includes asking patients about
the primary signs of heart failure and their medical history. A complete
physical examination includes venous pressure and functioning of the
lungs and heart. Laboratory tests to diagnose heart failure are electrocardiogram,
chest x-ray, echocardiography, exercise testing and levels of B-type
natriuretic peptide.
The diagnosis of heart failure is difficult because the presentation
of heart failure can change from patients with no symptoms to those
with pulmonary edema and cardiogenic shock. Only 50% of patients
with heart failure are diagnosed initially. Dr. Ventura discussed
a systematic approach to improve the diagnosis of heart failure.
This approach consists of clinical history, physical exam and laboratory
tests.
Clinical History
・ Primary signs of heart failure: dyspnea on exertion,
orthopnea, paroxysmal
nocturnal dyspnea,
fatigue, weakness
・ Patient medical history
・ Family medical history
|
Physical Examination
・ Complete physical examination
・ Venous pressure
・ Lung examination
・ Heart examination
|
|
Laboratory Tests
・ EKG
・ Chest radiograph
・ 12-lead echocardiography
・ Cardiopulmonary stress test
|
Blood Chemistry
・ B-type natriuretic peptide
・ Complete blood count
・ Urinalysis
・ Blood urea nitrogen
・ Liver and renal function tests
・ Thyroid stimulating hormone
・ Blood glucose
・ Serum creatinine
|
A complete clinical history includes asking patients about the
cardinal signs of heart failure: dyspnea on exertion, orthopnea,
paroxysmal nocturnal dyspnea, fatigue and weakness. As heart failure
progresses, patients may present with gastrointestinal problems
such as abdominal pain and distention. In late stages of heart failure,
neurological symptoms are present including anxiety or panic attacks,
syncope, decreased mental activity or confusion. Patients should
be asked about their history of hypertension, coronary artery disease,
myocardial infarctions and familial history of heart failure.
The second step in diagnosing heart failure is a complete physical
examination. Particular attention is given to venous pressure, the
lungs and heart. Venous pressure is checked by the hepatojugular
reflex. Breathing disorders, such as apnea/hypopnea and central
sleep apnea, are common in patients with heart failure. The heart
responds to the valsalva manuver in a characteristic manner in heart
failure.
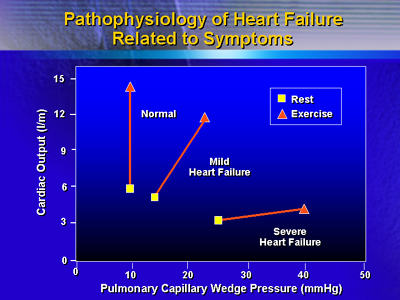
Laboratory tests used to diagnose heart failure are electrocardiogram,
chest x-ray, echocardiography, exercise testing, levels of B-type
natriuretic peptide and complete blood chemistries. The chest x-ray
is used to see the size of the heart and the pulmonary vasculature.
Echocardiography provides information on the structure and function
of the heart. Exercise or a cardiopulmonary stress test is used
because patients with heart failure have a decreased cardiac output,
pulmonary capillary wedge pressure, maximal oxygen consumption and
anaerobic threshold. B-type natriuretic peptide is an indicator
of the severity of heart failure.
Prognosis can be predicted from physical signs, B-type natriuretic
peptide and maximal oxygen consumption. Poor prognosis is indicated
by elevated venous pressure, third heart sounds, B-type natriuretic
peptide levels more than 73 pg/mL and maximal oxygen consumption
less than 14 mL/kg/min.
|