|
Protagonist:
Antiarrhythmic drug therapy for paroxysmal atrial fibrillation is
generally inadequate. Most cases arise from electrophysiologic sources
in the pulmonary veins. Ablation of focal source areas or a more general
blockade of electrophysiologic connections between the pulmonary vein
and the atrium are much more successful, producing cure rates as high
as 80%.
Antagonist: It is not appropriate
at this time to recommend pulmonary vein ablation for all patients
with paroxysmal atrial fibrillation. The procedure is associated
with risk of potentially severe adverse events including stroke,
cardiac tamponade, and pulmonary vein stenosis. Proper selection
and administration of antiarrhythmic drug therapy can treat these
patients with equivalent efficacy and better safety.
Protagonist: There are many problems associated with antiarrhythmic
drug therapy for atrial fibrillation. The simple fact is, drugs
don't work very well: many common drugs such as amiodarone, propafenone,
sotalol, are associated with a 60% probability of recurrence within
a year. The recurrence rate with amiodarone is lower, but few patients
are likely to take amiodarone for as long as 2 to 3 years. In fact,
when we do clinical trials to evaluate efficacy of antiarrhythmic
drugs, we measure average time between recurrences rather than cure
rates, because there are no cures. In addition, these drugs tend
to have high rates of side effects, which can dramatically reduce
the patients' quality of life. Also, many antiarrhythmics have a
significant pro-arrhythmic potential. Finally, these drugs tend
to be expensive. All of these factors have an adverse impact on
the patient's compliance with the prescribed medication regimen.
Atrial fibrillation is initiated by premature atrial events that
most typically occur in the pulmonary veins. Ablation techniques
have, therefore, focused on ablation of tissue in the pulmonary
veins. There are 2 general types of techniques: focal ablation of
the sites of abnormal activity, and a more empiric general approach
in which the pulmonary vein is broadly separated, in terms of electrophysiology,
from the atrium, essentially blocking potential arrhythmogenic activity
from reaching the atrium.
With either the older focal approach or the more recent pulmonary
vein isolation procedure, cure rates for patients with paroxysmal
atrial fibrillation are very good: about 70% with the older focal
procedure, and about 80% with the newer approach. Even for patients
with chronic or persistent atrial fibrillation, cure rates with
these approaches range from 20% to 60%, and typically reach the
50% to 60% range.
Interestingly, those patients who are not cured by the ablation
procedures tend to have excellent responses to subsequent pharmacologic
therapy. Therefore, the overall success rate of these procedures
is really in the 90% range.
Antagonist: It is very difficult for me to agree with a
recommendation for the use of pulmonary vein ablation for all patients
with paroxysmal atrial fibrillation. First, not all patients have
similar pathophysiology - we don't necessarily know the underlying
cause of atrial fibrillation in patients with congestive heart failure
or other underlying cardiovascular diseases. Second, the ablation
procedure carries significant risks. And third, when properly used,
drug therapy can provide equivalent efficacy and safety.
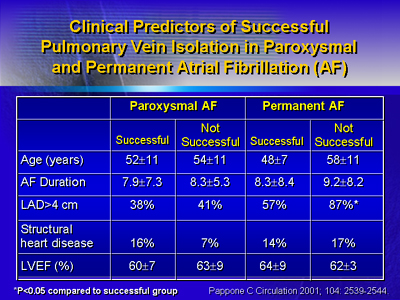
Most of the published data on the pulmonary vein ablation procedure
are from series of patients with an average age below 65, and with
cardiac ejection fractions well in the normal range. We have to
be careful about extrapolating these data to typical atrial fibrillation
patients who are 75 years old or have congestive heart failure.
While cure rates generally in the 65% to 75% range, and even as
high as 92%, are being seen with pulmonary vein ablation in electrophysiology
labs around the world, these procedures are associated with significant
adverse events rates of 2% to 3%. The adverse events include cerebrovascular
events, pericardial effusion and tamponade, and pulmonary vein stenosis.
In fact, a new clinical syndrome has been defined recently: pulmonary
vein stenosis following pulmonary vein ablation.
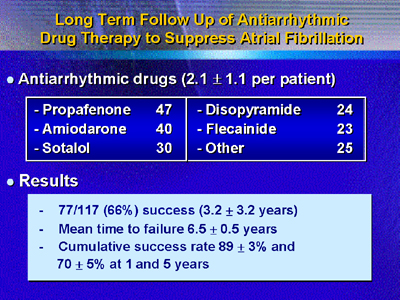
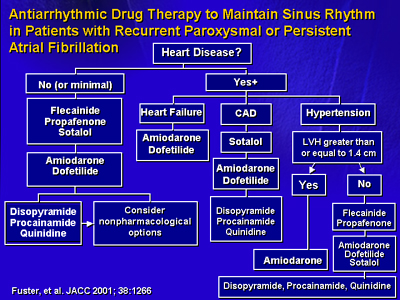
I have recently analyzed data from patients I have treated for
atrial fibrillation with antiarrhythmic drug therapy during the
last 15 years. By using an algorithmic approach to drug selection,
I have produced a success rate of 66% at 3.2 years of follow-up.
This is comparable to success rates reported with pulmonary vein
ablation, but such reports include follow-up times ranging from
4 months to 13 months, and no longer. The mean time to failure for
my patients was 6.5 years, and cumulative success rates with patients
being under good control were 89% at 1 year and 70% at 5 years.
Among these patients there were no cases of stroke, tamponade, or
pulmonary vein stenosis. Therefore, I cannot at this time recommend
pulmonary vein ablation for all patients with paroxysmal atrial
fibrillation.
|